- Strategies resulted in long-lasting improvements in both GI symptoms and quality of life (QOL).
- The multicomponent comprehensive self-management (CSM) program allowed patients to select the most effective and feasible strategies to self-manage symptoms.
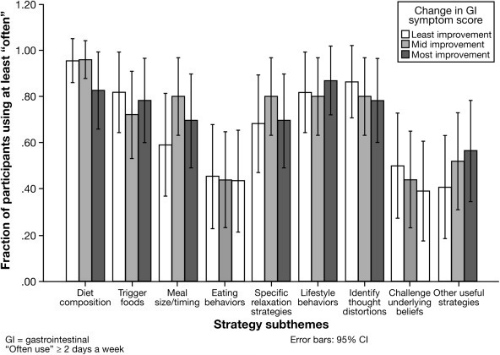
- Strategies included variations in diet, relaxation techniques, and tools for identifying thought distortions, and challenging underlying beliefs, among others.
- At 12 months’ follow-up after the CSM program, 94% of the participants (76/81) were still using ≥6 strategies and adherence was >79% for all subthemes of CMS strategies.
Comprehensive self-management (CSM) strategies are sustainable and effective for symptom control in patients with irritable bowel syndrome (IBS), according to results of a randomized trial published recently in Clinical Gastroenterology and Hepatology.
The Analysis
The researchers categorized CSM strategies from a previous clinical trial as diet (composition, trigger foods, meal size or timing, and eating behaviors), relaxation (specific relaxation strategies and lifestyle behaviors), and alternative thoughts (identifying thought distortions, challenging underlying beliefs, and other strategies). They then followed 81 adults with IBS (87% female; mean age 45 years) who had participated in the previous intervention trial.
This cohort study relied on follow-up data from a previous randomized trial of in-person or telephone CSM intervention versus usual care for adults with IBS. Of the participants 80% (101/126 participants) were randomly assigned to receive CSM intervention. This group completed a comprehensive plan at their final CSM session and were rolled into the current study. Of these, 80% (n=81) provided 12-month follow-up data.
The study included personal contact with a nurse therapist. This “might have also contributed to the high adherence rates,” the authors noted. “Patients with IBS were provided reassurance that they were correctly performing CSM strategies by observed practice and real-time feedback. Participants also received scheduled calls by our nurse therapist at 6 and 12 months. Such a call might have offered encouragement and support to the participant, resulting in increased adherence to behavioral changes as seen in other patient populations. This effect might have been even more pronounced in this study because participants had established relationships with these therapists,” they noted.
Methods
The CSM program was delivered in 9 sessions (1 hour each) over a 13-week period by 2 trained psychiatric nurse therapists. CSM sessions covered 3 main themes: (1) diet, (2) relaxation, and (3) alternative thoughts. Specific strategies within each main theme were selected for each participant based on individualized assessments by the nurse therapist. As the final homework assignment, participants were asked to write a comprehensive plan that specified which strategies they found the most helpful and planned on using over the next year in managing their IBS symptoms.
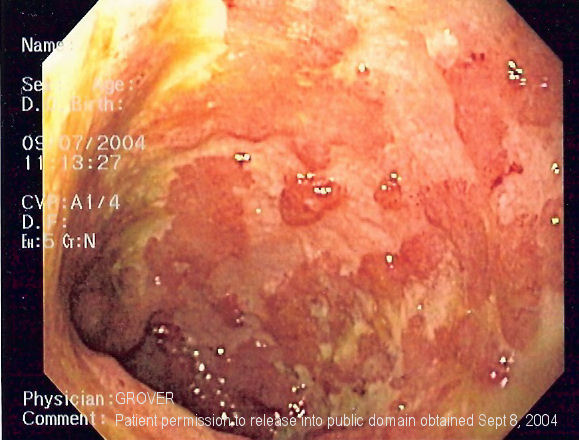
from ulcerative colitis due to the lack of superficial ulceration in IBS
Conclusions
At the last CSM session of the trial, 95% of the patients selected the subthemes of specific relaxation strategies, 90% selected diet composition, and 90% identified thought distortion strategies for continued use. At 12 months’ follow-up after the CSM program, 94% of the participants (76/81) were still using ≥6 strategies and adherence was >79% for all subthemes of CMS strategies.
Completion of the CSM program resulted in sustained health changes. At 12 months, a large majority of participants were still using CSM strategies. “The high adherence rates reported in this study were likely attributable to the unique structure of our CSM program, which offered flexibility, individualization, practice, and personal feedback,” the authors explained. “Our CSM program gave participants the freedom to pick and choose which strategies to use.”
The relatively high rates of adherence may have contributed to the lasting improvements seen in both symptoms and QOL in the parent study. In that study, 40% of participants had ≥50% improvement in GI symptoms at 12 months. Further analysis showed that 84% of participants demonstrated at least some improvement in GI symptom scores.
“Our CSM program resulted in sustainable behavioral changes for IBS symptom management in most of our participants, possibly accounting for the long-lasting improvements seen in both GI symptoms and QOL. A multicomponent CSM intervention allowed patients to select the most effective and feasible strategies for their individualized set of symptoms,” the authors concluded.
