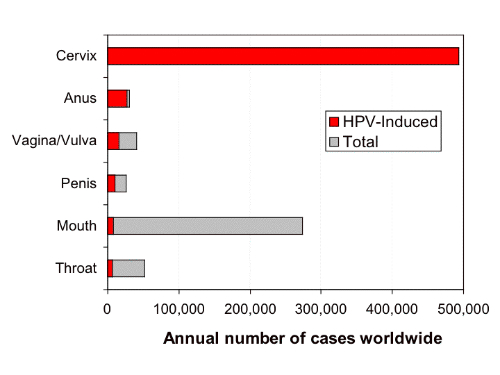
- Human papillomavirus (HPV) causes approximately 1.6% of the more than 1.6 million cases of cancer diagnosed in the U.S. each year.
- HPV the most common sexually transmitted infection.
- A highly effective vaccine is available to protect against HPV infection.
- Only about 38% of eligible females and 14% of eligible males receive the vaccine.
- Higher rates of adherence to CDC vaccination guidelines could significantly reduce the rate of HPV-related cancers.
Human papillomavirus (HPV) causes approximately 1.6% of the more than 1.6 million cases of cancer diagnosed annually in the U.S. each year. This is more than 25000 cancers that could be easily prevented each year by adherence to the vaccination protocol called for by the Centers for Disease Control and Prevention (CDC). Few medical interventions are as effective and cost-effective as is HPV vaccination.
Cost-Effectiveness
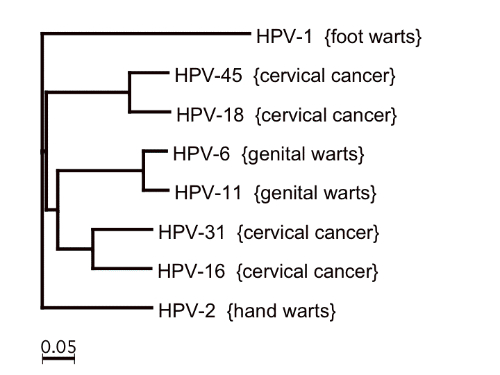
Available vaccine protocols have been shown to be safe and effective, yet HPV remains the most common sexually transmitted infection. “Underlying the high prevalence of HPV infection is the poor adherence to the Centers for Disease Control recommendation to vaccinate all 11- to 12-year-old males and females,” according to a report published recently Journal of Managed Care Pharmacy (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4682020) In the more than 10 years since the vaccines have become available only approximately 38% of eligible females and just 14% of eligible males receive the complete, 3-dose immunization, according to the authors of the report.
In fact, clinical studies have shown HPV vaccination to be highly effective and potentially lifesaving intervention if administered to females naive or unexposed to vaccine HPV types,” according to a review of 11 cost-effectiveness studies published in the Journal of Managed Care Pharmacy (http://www.amcp.org/data/jmcp/217-230.pdf).
Modeling studies have also shown that HPV vaccination can be cost-effective with an incremental cost-effectiveness ratio (ICER) of ≤$100,000 per quality adjusted life year (QALY) gained if administered to 12-year-old girls in the context of cervical screening intervals >1 year. “Catch-up vaccination through 21 years of age increases the cost per QALY to more than $100,000. Until real-world coverage rates increase, cost-effectiveness modeling of HPV vaccination underestimates the actual cost per QALY,” according to the article in the Journal of Managed Care Pharmacy.
Why Low Compliance?
Many factors appear to be causing the low rates of HPV vaccination. According to the authors of the article in the Journal of Managed Care Pharmacy, may factors contribute to the widespread disparities in vaccine completion and related health outcomes. These include race, age, family income, and patient education.
Responsibility Falls on Primary Care Physicians
The rigor and consistency of recommendations of HPV vaccination by primary care physicians (PCPs) plays a significant role in in the rate of HPV immunization. Health disparity data are vitally important to HPV vaccination campaigns because they can show PCPs how to address the low rates of vaccination and urge PCP practices to allocate resources in ways to improve the rates. Even modest improvements in vaccination rates among populations where they are low would yield significantly benefits. HPV immunization has been shown to provide herd immunity thereby protecting non-immunized individuals.

“However, the impact of current HPV vaccination campaigns is hindered by stagnant immunization rates, which remain far below target levels despite a slow overall increase. Furthermore, gains in immunization are not equally distributed across gender, age, demographic, and socioeconomic divisions within the recommended group of vaccine recipients” according to the authors of the report in the Journal of Managed Care Pharmacy.
“To achieve the greatest impact, public health campaigns should focus on improving immunization coverage where it is weakest. They should also explore more subtle but potentially significant determinants of HPV vaccine initiation and completion, such as the attitudes of parents and healthcare providers and factors that exacerbate HPV-related health outcomes, including smoking and human immunodeficiency virus (HIV)-mediated immunosuppression. Optimizing the efficacy of vaccination campaigns will require a health disparities approach that both identifies and remedies the underlying causes of population differences in HPV vaccination” they concluded.
