- Homogeneous gut microbial population (dysbiosis) is associated with increased risk of allergies and other adverse conditions.
- Analysis based on data from the American Gut Project and fecal 16S rRNA sequence data.
- The researchers examined 122 non-redundant taxa (of 2379 total taxa) with a ≥0.1% mean abundance in calculating microbiota richness and diversity.
- Reduced fecal microbial diversity was associated with increased rates of allergy to foods (peanuts, tree nuts, shellfish, other) and non-foods (drug, bee sting, dander, asthma, seasonal, eczema).
- Findings appear to provide further support to the hygiene hypothesis of allergy and autoimmunity.
- Dysbiosis might be targeted with bacteriotherapy to improve treatment or prevention of a wide variety of allergies.
Allergies, specifically type I hypersensitivity disorders, are clinically important and increasingly prevalent among U.S. adults. Between 1988–1994 and 2005–2006, the prevalence of physician-diagnosed seasonal pollen allergy (hay fever), for example, increased from 8.8% to 11.3%. The prevalence of asthma among the U.S. population in 2005–2006 was estimated to be 14.1%. Modern hygiene has been postulated to contribute to the increasing prevalence of allergies, based on both functional and observational studies.
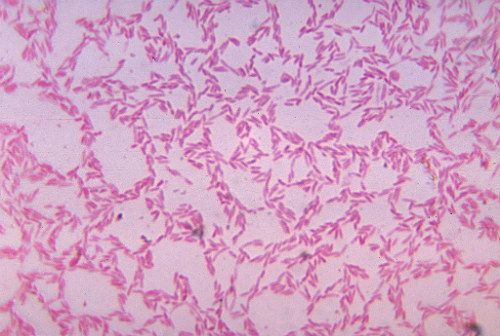
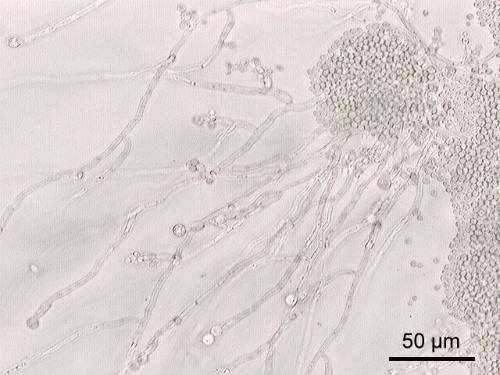
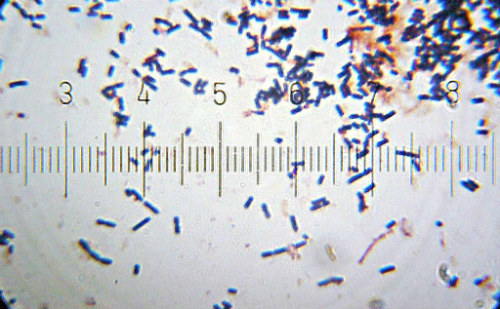
Alteration of the gut microbial population (dysbiosis) may increase the risk of allergies and other conditions, according to the results of a study published recently in EBioMedicine. The study included an analysis of data from the American Gut Project. Bacteriotherapy (Figure 1) may be an effective intervention for clinically significant dysbiosis if important microbes (Figures 2-6) are reintroduced into the gut.
.jpg)
The Analysis
The researchers analyzed publicly available data from the American Gut Project questionnaire and from fecal 16S rRNA sequencing. Fecal microbiota richness (number of observed species), diversity, and composition (UniFrac; UniFrac is a distance metric used for comparing biological communities. It differs from distance metrics such as Bray-Curtis dissimilarity in that it incorporates information on the relative relatedness of community members by incorporating phylogenetic distances between observed organisms in the computation.) were used to compare adults with and without allergies to foods (peanuts, tree nuts, shellfish, and others), as well as non-food allergies (drug, bee sting, dander, asthma, seasonal, eczema).
The researchers employed logistic and Poisson regression models in order to adjust for potential confounders. They calculated odds ratios (OR) and 95% confidence intervals (CI) for lowest vs highest fecal microbiota richness, including 122 non-redundant taxa (of 2379 total taxa).
Results
The study included 1879 participants (mean age, 45.5 years; 46.9% male). The self-reported allergy prevalence among this population was 81.5%. The incidence ranged from 2.5% for peanut allergies to 40.5% for seasonal allergies.
Fecal microbiota richness was markedly lower among participants who reported total allergies (P=10 [-9]) and 5 particular allergies (P≤10 [-4]). Richness odds ratios were 1.7 (CI 1.3-2.2) among participants who reported seasonal allergies, 1.8 (CI 1.3-2.5) among those who reported drug allergies, and 7.8 (CI 2.3-26.5) among those with peanut allergy.
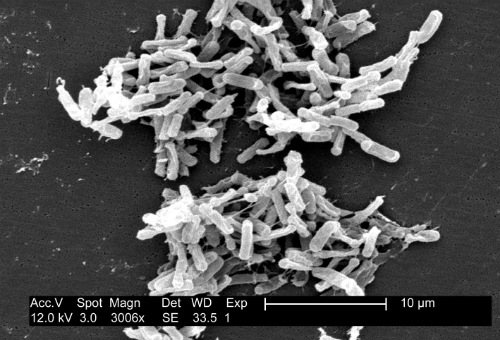
Participants who reported having allergy also demonstrated markedly altered microbial community composition (unweighted UniFrac, P=10[-4] to 10[-7]), the researchers reported. Total food and non-food allergies were significantly associated with 7 and 9 altered taxa, respectively. The dysbiosis was most marked among participants who reported nut and seasonal allergies. This phenomenon may have been driven by higher Bacteroidales and reduced Clostridiales taxa, the authors explained.
The Hygiene Hypothesis
These results appear to lend additional support to the hygiene hypothesis which states that a lack of early childhood exposure to infectious agents, symbiotic microorganisms (such as the gut flora or probiotics), and parasites, increases susceptibility to allergic diseases by suppressing the natural development of the immune system. (See our related article here.)
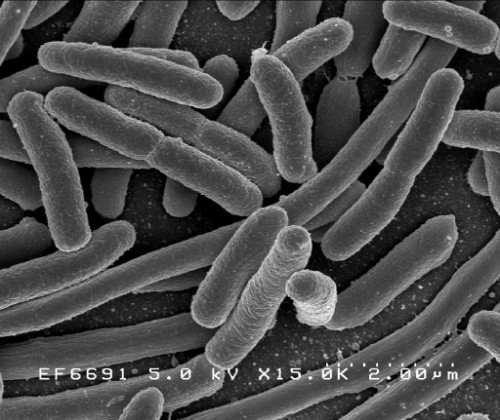
Figure 5. Escherichia Coli.
Conclusions
“American adults with allergies, especially to nuts and seasonal pollen, have low diversity, reduced Clostridiales, and increased Bacteroidales in their gut microbiota. This dysbiosis might be targeted to improve treatment or prevention of allergy,” the researchers concluded.
