- Synthetic mesh reinforcement had an expected cost of $15,776 and quality-adjusted life-year value gained of 21.03.
- Biological mesh had an expected cost of $23,844 and quality-adjusted life-year value gained of 20.94.
- Monte Carlo sensitivity analysis demonstrated that synthetic mesh was the preferred and most cost-effective strategy in 94 percent of simulations, supporting its overall greater cost-utility.
- Despite varying the willingness-to-pay threshold from $0 to $100,000 per quality-adjusted life-year, synthetic mesh remained the optimal strategy across all thresholds in sensitivity analysis.
Synthetic mesh repair of clean-contaminated hernias is more cost-effective than repair with acellular dermal matrix, according to a systematic review published recently in Plastic and Reconstructive Surgery.

However, the efficacy of the various types of mesh is not well understood. This is particularly true in patients with contaminated hernia defects.
Mesh Repair: The Evidence
A prospective study of 85 patients published in Surgery in 2012, found that the use of the intact, non-cross-linked, porcine, acellular dermal matrix, Strattice, in the repair of contaminated ventral incision hernia in high-risk patients resulted in successful, single-stage reconstruction in >70% of patients followed for 24 months.
A 2012 systematic review published in the World Journal of Surgery found that mesh repair significantly reduced the number of recurrences. However, in patients without recurrence mesh repairs appeared to be associated with an increased risk of chronic pain especially if the mesh is fixed sublay, the authors noted.
However, a prospective study of more than 33,000 cases published the Annals of Surgery in 2012, resulted in a contradictory finding. “There is a significant increase in risk of postoperative occurrences following VHRs using mesh in clean-contaminated and contaminated cases relative to clean cases. We recommend avoiding the use of mesh in any level of contamination,” the authors concluded.
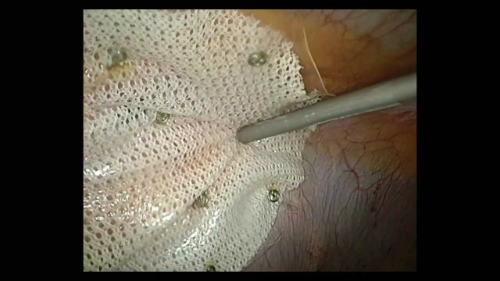
“Acellular dermal matrix has enabled single-stage ventral hernia repair in clean-contaminated wounds but can be associated with higher complications and cost compared with synthetic mesh. This study evaluated the cost-utility of synthetic mesh and acellular dermal matrix for clean-contaminated ventral hernia repairs” the authors explained.
Types of Mesh: The Analysis
The 2016 systematic review published in Plastic and Reconstructive Surgery compared outcomes for hernia repair with synthetic versus biologic acellular dermal matrix mesh. The authors evaluated quality-adjusted life years (QALYs) using a Web-based visual analog scale survey of 300 nationally representative individuals. Overall expected cost and QALYs for ventral hernia repair were assessed using a Monte Carlo simulation with sensitivity analyses.

The Results
Synthetic mesh reinforcement had an expected cost of $15,776 and QALY value gained of 21.03. In contrast, biological mesh repairs resulted in an expected cost of $23,844 and QALY value gained of 20.94.
When the authors referenced a common baseline, a do nothing strategy, acellular dermal matrix and synthetic mesh were judged cost-effective, although synthetic mesh was more strongly favored. Biologic mesh repairs resulted in incremental cost-effectiveness ratio of $3378 ($/QALYs). Synthetic mesh repairs performed better with an incremental cost-effectiveness ratio of $2208 ($/QALYs).
The authors also performed a Monte Carlo sensitivity analysis which demonstrated that synthetic mesh was the preferred and most cost-effective strategy in 94% of simulations, thereby supporting its overall greater cost-utility.
“This cost-utility analysis suggests that synthetic mesh repair of clean-contaminated hernia defects is more cost-effective than acellular dermal matrix,” the reviewers concluded.
