- Evidence of risks associated with proton pump inhibitors continues to accumulate.
- Proton pump inhibitors may be overprescribed in place of lifestyle modifications.
- Risk of chronic kidney disease is added to risk of gastrointestinal tract hemorrhage and infectious complications in the intensive care unit potentially attributable to PPI use.
- No causal mechanisms of potential PPI injury have been identified.
Proton pump inhibitor (PPI) use was associated with a higher risk of developing chronic kidney disease (CKD), according to a recent report in JAMA Internal Medicine. The study did not establish a causal link between PPI use and CKD but the authors called for additional research to examine the relationship.
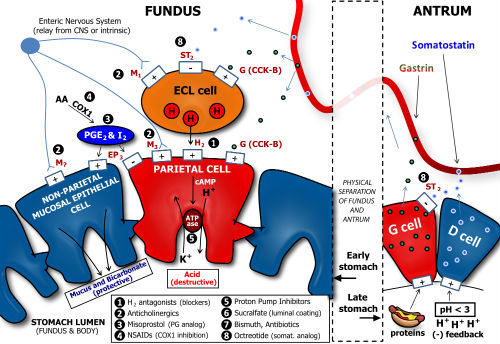
Figure 1. Diagram depicting the major determinants of gastric acid secretion, with inclusion of drug targets for peptic ulcer disease (PUD) and gastroesophageal reflux disease (GERD).
Study Structure
The study included 10,482 participants in the Atherosclerosis Risk in Communities study who had an estimated glomerular filtration rate (GFR) of ≥60 mL/min/1.73 m2. Patients were followed from an initial baseline between 1996 and 1999 visit for approximately 15 years to late 2015. “The findings were replicated in an administrative cohort of 248,751 patients with an estimated glomerular filtration rate of at least 60 mL/min/1.73 m2 from the Geisinger Health System,” the authors wrote.
The researchers estimated that over 10 years, the absolute risk of developing CKD among the Geisinger patients was 15.6% among PPI users, but just 13.9% among non-users. Participants in the Atherosclerosis Risk in Communities study had a mean age of 63.0 years and 43.9% were male. Compared with nonusers, PPI users were more often white, obese, and taking antihypertensive medication.
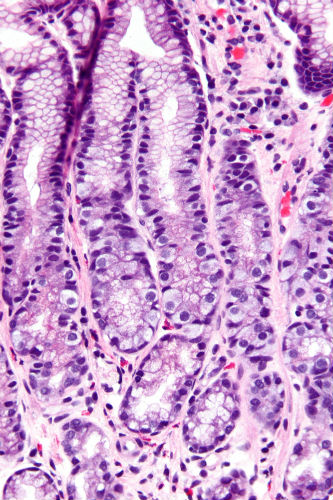
Figure 2. Micrograph of the gastric antrum showing G-cell hyperplasia, a histomorphologic change seen with PPI use (H&E stain).
Results and Conclusions
Proton pump inhibitor use was associated with CKD in both unadjusted analysis (hazard ratio [HR], 1.45; 95% CI, 1.11-1.90) and in analysis adjusted for demographic, socioeconomic, and clinical variables (HR, 1.50; 95% CI, 1.14-1.96). The association persisted when baseline PPI users were compared directly with H2 receptor-antagonist users (adjusted HR, 1.39; 95% CI, 1.01-1.91) and with propensity score-matched nonusers (HR, 1.76; 95% CI, 1.13-2.74).
In the Geisinger Health System replication cohort, PPI use was associated with CKD in all analyses, including a time-varying new-user design (adjusted HR, 1.24; 95% CI, 1.20-1.28). Twice-daily PPI dosing (adjusted HR, 1.46; 95% CI, 1.28-1.67) was associated with a higher risk than once-daily dosing (adjusted HR, 1.15; 95% CI, 1.09-1.21).
JAMA Internal Medicine Accompanying Editorial
“Proton pump inhibitors (PPIs) have been among the most widely prescribed medications in the United States for decades. This is largely due to 2 very common uses of PPIs: treatment of dyspepsia and prevention of gastrointestinal bleeding among patients prescribed antiplatelet therapy, coupled with the belief that PPIs have few adverse effects. However, mounting evidence) demonstrates that PPIs are associated with a number of adverse effects and are overprescribed.
“This issue was highlighted in JAMA Internal Medicine’s launch of the Less Is More series in 2010. Since then, additional evidence of adverse effects of PPIs has accumulated. In this issue of JAMA Internal Medicine, Lazarus et al add chronic kidney disease to the list of possible harms of PPIs,” Adam Jacob Schoenfeld, MD and Deborah Grady, MD, MPH wrote in an editorial accompanying the report by Lazarus et al.
“Many patients with heartburn and indigestion don’t need PPIs,” Dr. Schoenfeld told Reuters Health. “Behavior and lifestyle changes such as getting more exercise and drinking less alcohol may have the same effect as PPIs for mild stomach symptoms.”
