- Of the 18.5 million Part D beneficiaries receiving hypertensive medications 4.9 million (26%) were nonadherent in 2014, according to Centers for Disease Control and Prevention.
- Medicare Part D beneficiaries pegged as particularly nonadherent.
- Misuse of antihypertensives constitutes an important expenditure of national health funds.
- Nonadherence is linked to significant cardiovascular disease.
Nonadherence to prescribed antihypertensive regimens is identified as a leading cause of poor blood pressure control among hypertensive patients and an important risk factor for adverse cardiovascular disease outcomes (Figure 1), according to a recent report in Mortality and Morbidity Weekly Report (MMWR). Of the 18.5 million Medicare Part D beneficiaries who are prescribed antihypertensives 4.9 million (26%) were non adherent in 2014, according to The Centers for Disease Control and Prevention (CDC).
“Nonadherence to taking prescribed antihypertensive medication (antihypertensive) regimens has been identified as a leading cause of poor blood pressure control among persons with hypertension and an important risk factor for adverse cardiovascular disease outcomes. CDC and the Centers for Medicare and Medicaid Services analyzed geographic, racial-ethnic, and other disparities in nonadherence to antihypertensives among Medicare Part D beneficiaries in 2014,” the CDC authors wrote in MMWR.
“Antihypertensive nonadherence, defined as a proportion of days a beneficiary was covered with antihypertensives of <80%, was assessed using prescription drug claims data among Medicare Advantage or Medicare fee-for-service beneficiaries aged ≥65 years with Medicare Part D coverage during 2014 (N = 18.5 million). Analyses were stratified by antihypertensive class, beneficiaries’ state and county of residence, type of prescription drug plan, and treatment and demographic characteristics,” they added.
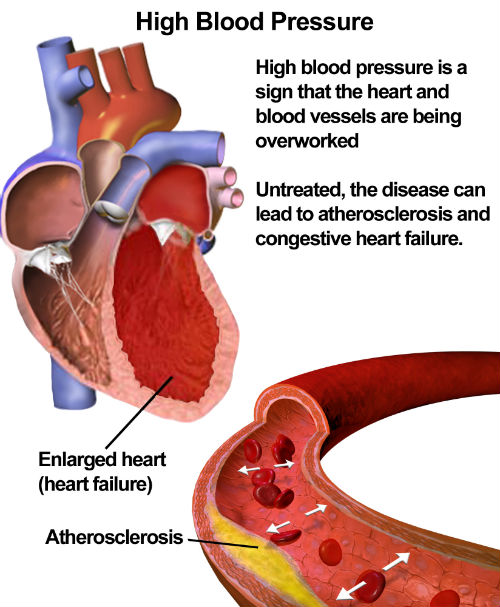
(Sources: Wikipedia/By Blausen.com staff. "Blausen gallery 2014"/Creative Commons.)
The Data
- The researchers found that about 26.3% (4.9 million) of Medicare Part D beneficiaries using antihypertensives (Figure 2) were nonadherent to their regimen. Nonadherence differed by multiple factors:
- Medication class (range: 16.9% for angiotensin II receptor blockers to 28.9% for diuretics)
- Race-ethnicity (24.3% for non-Hispanic whites, 26.3% for Asian/Pacific Islanders, 33.8% for Hispanics, 35.7% for blacks, and 38.8% for American Indians/Alaska Natives)
- State of residence (range 18.7% for North Dakota to 33.7% for the District of Columbia).
- Considerable county-level variation in nonadherence was found; the highest nonadherence tended to occur in the southern United States (U.S. Census region nonadherence = 28.9% [South], 26.7% [West], 24.1% [Northeast], and 22.8% [Midwest])
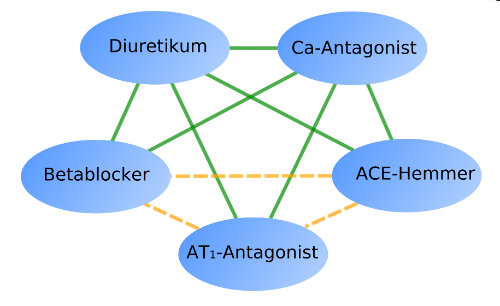
(Sources: Wikipedia/By PhilippN/GNU Free/Creative Commons.)
The Analysis
Physicians must be aware that more than one in four Medicare Part D beneficiaries using antihypertensives is nonadherent to the antihypertensive regimen. Certain racial/ethnic groups, states, and geographic areas are at increased risk for nonadherence.
These data offer physicians a patient group upon which to focus with increased education and facilitation of antihypertensive regimens to which adherence is easier. By focusing on these groups physicians can significantly reduce the risk of negative cardiovascular sequelae and resulting morbidity and mortality.
By identifying these patients and spending additional time with them in education and understanding the barriers to adherence, physicians can help to significantly reduce national health-related expenditures. The U.S. is a world leader in hypertension and related cardiovascular morbidity and mortality (Figure 3).
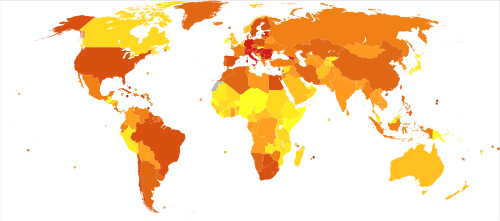
(Darker colors indicate higher rates.)
(Sources: Wikipedia/By Chriss55/Creative Commons.)
Key Points from the CDC:
- Cardiovascular disease (heart disease and stroke) is the leading cause of death in the United States.
- Hypertension, or high blood pressure, is a primary risk factor for heart disease and stroke, and approximately 70% of adults aged ≥65 years have the condition. Only about half of persons with high blood pressure have it under control (i.e., blood pressure <140/90 mm Hg).
- Nonadherence, or not following a health care professional’s instructions concerning taking their prescribed blood pressure medicine, is a well-known reason for uncontrolled high blood pressure and an important risk factor for adverse cardiovascular disease outcomes and increased health care costs.
- In this study, 26.3% (4.9 million) Medicare Part D beneficiaries aged ≥65 years using blood pressure medicine were considered nonadherent.
- Different groups and geographic regions had a high proportion of beneficiaries classified as nonadherent. For example, 24.3% of whites, 26.3% of Asian/Pacific Islanders, 33.8% of Hispanics, 35.7% of blacks, and 38.8% of American Indians or Alaska Natives were classified as being nonadherent. In addition, socioeconomic status classifications showed differences, with 32.1% of persons with a low-income subsidy being classified as nonadherent, compared with 25.4% of persons with no subsidy. The highest nonadherence prevalence tended to occur in the southern United States.
- Factors and opportunities were identified that could be addressed by prescribers, health systems, and payers to improve adherence, including, especially among older adults, simplifying their blood pressure medication regimen.
