- The American Pain Society (APS) has issued new guidelines for the management postoperative pain.
- While the new guidelines address postop pain specifically, they can be beneficial for patients with both acute and chronic pain.
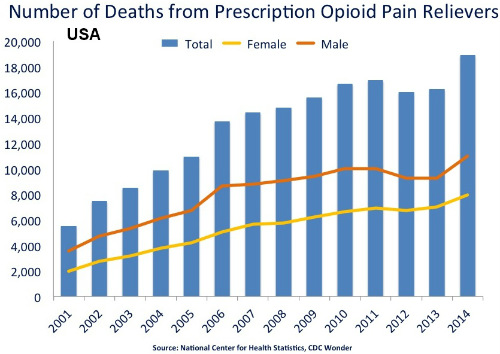
- The guidelines were clearly drawn with an eye on the opioid abuse epidemic that continues in the U.S.
- The APS recommends a multimodal analgesic approach in all appropriate cases.
- The multimodal approach includes reduce use of opioid analgesics and reduced duration of use when opioids are clinically appropriate.
The American Pain Society has issued 32 new guidelines intended to improve the management of postoperative pain. The guidelines were published in The Journal of Pain.
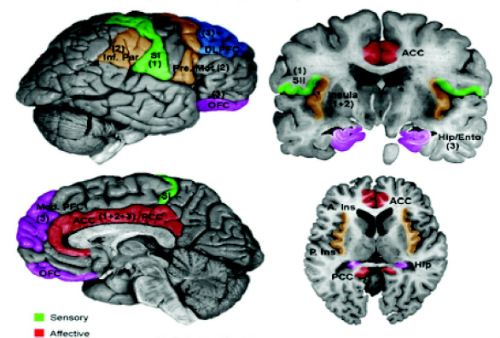
of cortical areas involved with pain processing.
Overview
The APS convened a multidisciplinary expert panel to develop new clinical practice guidelines for evidence-based, effective, and safer management of postoperative pain in children and adults. The APS joined forces with the American Society of Anesthesiologists and the American Society for Regional Anesthesia.
The authors formulated 32 recommendations for various aspects of postoperative pain management based on a systematic review of available evidence. The recommendations include direction on preop education, perioperative pain management planning, use of pharmacologic and nonpharmacologic modalities, organizational policies, and transition to outpatient care.
“Proper management of postoperative pain begins with an assessment of the patient in the preoperative period and development of a care plan specific to the individual and the surgical procedure involved. For many situations, evidence supports the use of multimodal regimens for pain management,” the authors wrote.
“Safe and effective postoperative pain management should be on the basis of a plan of care tailored to the individual and the surgical procedure involved, and multimodal regimens are recommended in many situations,” they added.
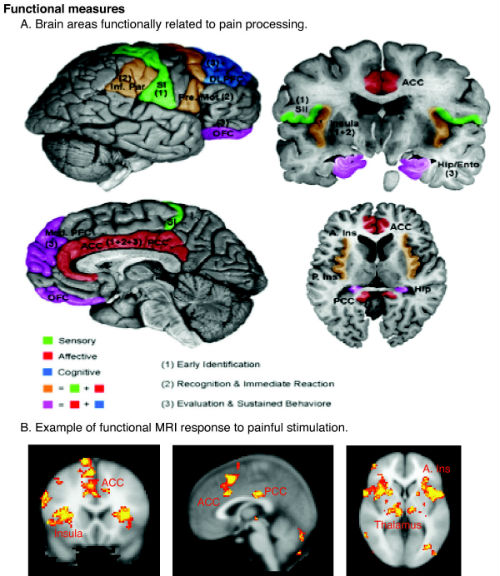
The highlighted areas summarize areas found active in previous functional imaging studies.
The APS made its recommendations with varying levels of fortitude and based them on evidence of varying quality. For a full explanation of the APS committee’s methodologies, visit the February 2016 issue of The Journal of Pain.
Recommendation 1
The panel recommends that clinicians provide patient and family-centered, individually tailored education to the patient (and/or responsible caregiver), including information on treatment options for management of postoperative pain, and document the plan and goals for postoperative pain management (strong recommendation, low-quality evidence).
Recommendation 2
The panel recommends that the parents (or other adult caregivers) of children who undergo surgery receive instruction in developmentally-appropriate methods for assessing pain as well as counseling on appropriate administration of analgesics and modalities (strong recommendation, low-quality evidence).
Recommendation 3
The panel recommends that clinicians conduct a preoperative evaluation including assessment of medical and psychiatric comorbidities, concomitant medications, history of chronic pain, substance abuse, and previous postoperative treatment regimens and responses, to guide the perioperative pain management plan (strong recommendation, low-quality evidence).
Recommendation 4
The panel recommends that clinicians adjust the pain management plan on the basis of adequacy of pain relief and presence of adverse events (strong recommendation, low-quality evidence).
Recommendation 5
The panel recommends that clinicians use a validated pain assessment tool to track responses to postoperative pain treatments and adjust treatment plans accordingly (strong recommendation, low quality evidence).
Recommendation 6
The panel recommends that clinicians offer multimodal analgesia, or the use of a variety of analgesic medications and techniques combined with nonpharmacological interventions, for the treatment of postoperative pain in children and adults (strong recommendation, high-quality evidence).
Recommendations 7 and 8
The panel recommends that clinicians consider transcutaneous electrical nerve stimulation (TENS) as an adjunct to other postoperative pain treatments (weak recommendation, moderate-quality evidence).
The panel can neither recommend nor discourage acupuncture, massage, or cold therapy as adjuncts to other postoperative pain treatments (insufficient evidence).
Recommendation 9
The panel recommends that clinicians consider the use of cognitive–behavioral modalities in adults as part of a multimodal approach (weak recommendation, moderate-quality evidence).
Recommendation 10
The panel recommends oral over intravenous (I.V.) administration of opioids for postoperative analgesia in patients who can use the oral route (strong recommendation, moderate quality evidence).
Recommendation 11
The panel recommends that clinicians avoid using the intramuscular route for the administration of analgesics for management of postoperative pain (strong recommendation, moderate-quality evidence).
Recommendation 12
The panel recommends that I.V. patient-controlled analgesia (PCA) be used for postoperative systemic analgesia when the parenteral route is needed (strong recommendation, moderate-quality evidence).
Recommendation 13
The panel recommends against routine basal infusion of opioids with I.V. PCA in opioid-naive adults (strong recommendation, moderate-quality evidence).
Recommendation 14
The panel recommends that clinicians provide appropriate monitoring of sedation, respiratory status, and other adverse events in patients who receive systemic opioids for postoperative analgesia (strong recommendation, low-quality evidence).
Recommendation 15
The panel recommends that clinicians provide adults and children with acetaminophen and/or nonsteroidal anti-inflammatory drugs (NSAIDs) as part of multimodal analgesia for management of postoperative pain in patients without contraindications (strong recommendation, high-quality evidence).
Recommendation 16
The panel recommends that clinicians consider giving a preoperative dose of oral celecoxib in adult patients without contraindications (strong recommendation, moderate-quality evidence).
Recommendation 17
The panel recommends that clinicians consider use of gabapentin or pregabalin as a component of multimodal analgesia (strong recommendation, moderate-quality evidence).
Recommendation 18
The panel recommends that clinicians consider I.V. ketamine as a component of multimodal analgesia in adults (weak recommendation, moderate-quality evidence).
Recommendation 19
The panel recommends that clinicians consider I.V. lidocaine infusions in adults who undergo open and laparoscopic abdominal surgery who do not have contraindications (weak recommendation, moderate-quality evidence).
Recommendation 20
The panel recommends that clinicians consider surgical site–specific local anesthetic infiltration for surgical procedures with evidence indicating efficacy (weak recommendation, moderate-quality evidence).
Recommendation 21
The panel recommends that clinicians use topical local anesthetics in combination with nerve blocks before circumcision (strong recommendation, moderate-quality evidence).
Recommendation 22
The panel does not recommend intrapleural analgesia with local anesthetics for pain control after thoracic surgery (strong recommendation, moderate-quality evidence).
Recommendation 23
The panel recommends that clinicians consider surgical site–specific peripheral regional anesthetic techniques in adults and children for procedures with evidence indicating efficacy (strong recommendation, high-quality evidence).
Recommendation 24
The panel recommends that clinicians use continuous, local anesthetic–based peripheral regional analgesic techniques when the need for analgesia is likely to exceed the duration of effect of a single injection (strong recommendation, moderate-quality evidence).
Recommendation 25
The panel recommends that clinicians consider the addition of clonidine as an adjuvant for prolongation of analgesia with a single-injection peripheral neural blockade (weak recommendation, moderate-quality evidence).
Recommendation 26
The panel recommends that clinicians offer neuraxial analgesia for major thoracic and abdominal procedures, particularly in patients at risk for cardiac complications, pulmonary complications, or prolonged ileus (strong recommendation, high-quality evidence).
Recommendation 27
The panel recommends that clinicians avoid the neuraxial administration of magnesium, benzodiazepines, neostigmine, tramadol, and ketamine in the treatment of postoperative pain (strong recommendation, moderate-quality evidence).
Recommendation 28
The panel recommends that clinicians provide appropriate monitoring of patients who have received neuraxial interventions for perioperative analgesia (strong recommendation, low-quality evidence).
Recommendation 29
The panel recommends that facilities in which surgery Is performed have an organizational structure in place to develop and refine policies and processes for safe and effective delivery of postoperative pain control (strong recommendation, low-quality evidence).
Recommendation 30
The panel recommends that facilities in which surgery is performed provide clinicians with access to consultation with a pain specialist for patients with inadequately controlled postoperative pain or at high risk of inadequately controlled postoperative pain (eg, opioid-tolerant, history of substance abuse) (strong recommendation, low-quality evidence).
Recommendation 31
The panel recommends that facilities in which neuraxial analgesia and continuous peripheral blocks are performed have policies and procedures to support their safe delivery and trained individuals to manage these procedures (strong recommendation, low-quality evidence).
Recommendation 32
The panel recommends that clinicians provide education to all patients (adult and children) and primary caregivers on the pain treatment plan including tapering of analgesics after hospital discharge (strong recommendation, low-quality evidence).
