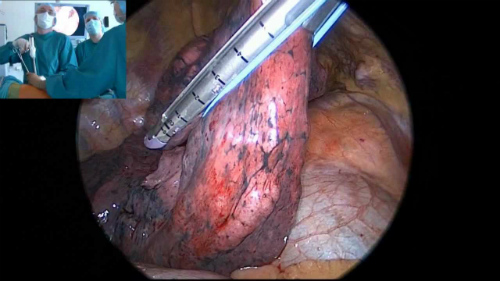
- The adequacy and efficacy of lobectomy and lymph node clearance are crucial to the survival of patients with non-small-cell lung cancer (NSCLC).
- Concern has been expressed as to whether patients are being understaged due to the inferior oncologic skill of these thoracic surgeons.
- Survival and recurrence rates are improved with institutional experience with VATS lobectomy.
The adequacy and efficacy of lobectomy and lymph node clearance are crucial to the survival of patients with non-small-cell lung cancer (NSCLC). Increasingly, video-assisted thoracic surgery (VATS) lobectomies are being performed by thoracic surgeons. Concern has been expressed as to whether patients are being understaged due to the inferior oncologic skill of these surgeons.
Paul Lee, MD, et al, undertook a retrospective study to assess the adequacy of lymph node clearance by VATS compared with thoracotomy, and the resulting accuracy of staging. “One factor that may be overlooked in published studies is the learning curve of the surgeons and surgical volume in the adoption of VATS lobectomy. This study examined the effect of cumulative institutional VATS lobectomy experience on the adequacy of lymphadenectomy,” wrote Lee et al in The Annals of Thoracic Surgery.
The researchers reviewed a prospective database to identify 500 consecutive patients who underwent VATS lobectomy for non-small cell lung cancer (NSCLC) at Weill Medical College of Cornell University between 2002 and 2012. For comparative purposes, the cohort was divided into halves, with an early group (the first 250 cases) versus a late group (the next 250 cases). “Clinical and pathologic factors were analyzed. A propensity-matching analysis controlling for age, gender, pathologic stage, and percentage of forced expiratory volume in 1 second was done to compare survival and adequacy of lymphadenectomy,” according to the abstract.
Significantly Improved Results Over Time
These researchers found that surgical results improved significantly over time; the second 250 cases were more difficult and still showed better results:
- Patients operated on in the late group were significantly older (72 vs 69 years, P=0.001).
- Had worse pulmonary functions (median forced expiratory volume in 1 second 83% vs 91%, P<0.001; median diffusion capacity of the lung for carbon monoxide, 76% vs 85%, P<0.001).
- Clinical and pathologic tumor sizes were significantly larger in the late group compared with the early group, with a median of 2.0 vs 1.8 cm (P= 0.002) for clinical T size and median of 2.1 vs 2.0 cm (P= 0.003) for pathologic T size.
- Patients in the late group had significantly more advanced clinical and pathologic stage distribution.
- The total number of lymph nodes and the number of nodal stations removed were significantly greater in the late group (P= 0.012) than in the early group (P<0.001), and same results were obtained after propensity matching.
- No difference was seen in disease-free survival between the propensity-matched early vs late groups at 3 years (82% vs 85%, P=0.187).
“For patients with NSCLC resected by VATS lobectomy, cumulative institutional experience significantly and positively affects the adequacy of lymphadenectomy,” the researchers concluded. “This may be related to the initial surgeon’s learning curve with VATS lobectomy. As the experience with VATS lobectomy becomes more mature, the procedure is increasingly being performed on older patients, often with more compromised pulmonary function and more advanced stage disease. Despite the expanded inclusion of older and sicker patients for VATS lobectomy, no compromise was seen in their disease-free survival,” they explained.
