- Study conducted by the National Health Service in Britain.
- Cost of biologics was seen as prohibitive.
- Initial treatment failed in patients with moderately to severely active ulcerative colitis.
- Infliximab, adalimumab and golimumab were superior to placebo for second-line therapy.
- Systematic review and network meta-analysis included 10 randomized, controlled trials (RCTs).
- Highly sophisticated statistical analysis included nearly 5000 patients.
- Cost effectiveness ratio modeling suggests that treatment with 1 of 3 monoclonal antibodies costs US$40,000 to nearly US$55,000 per quality-adjusted life-year (QALY) gained vs. colectomy.
Three monoclonal antibodies were found superior to colectomy for treatment of ulcerative colitis (Figure 1). However, cost was found to be prohibitive and the authors suggested that colectomy would continue to dominate as a clinical choice despite the general superiority of the biologic agents.
_active%20cropped.jpg)
a classic finding in ulcerative colitis.
(Sources: Wikipedia/Creative Commons.)
The systematic review and network meta-analysis, including 10 randomized, controlled trials (RCTs) and nearly 5000 patients. It was conducted by researchers within the National Institute for Health and Care Excellence (NICE) in the United Kingdom (UK) and published recently in Health Technology Assessment. The reviewers examined the clinical and cost effectiveness of adalimumab, golimumab, and infliximab versus colectomy and placebo. (Figure 2.)
Despite the apparent clinical superiority of the 3 biologic entities, the estimated incremental cost-effectiveness ratio (ICER) for infliximab—the most cost effective of the 3—versus standard non-biological treatment—colectomy—was estimated £37,682 per quality-adjusted life-year (QALY) gained. Patients included those for whom conventional therapies had failed.

with intractable ulcerative colitis. Colectomy specimen.
(Sources: Wikipedia/Photograph by Ed Uthman, MD.)
The Analysis
The reviewers searched the MEDLINE, EMBASE, Cumulative Index to Nursing and Allied Health Literature, The Cochrane Library including the Cochrane Systematic Reviews Database, Cochrane Controlled Trials Register, Database of Abstracts of Reviews of Effects, the Health Technology Assessment database and NHS Economic Evaluation Database; ISI Web of Science, including Science Citation Index, and the Conference Proceedings Citation Index-Science and Bioscience Information Service Previews databases for relevant studies. Included studies dated from the inception of the databases to December 2013 for clinical effectiveness searches and from inception to January 2014 for cost-effectiveness. They also performed searches of the US Food and Drug Administration and the European Medicines Agency websites, among other sources. They included RCTs and network meta-analyses.
The aim was to evaluate the clinical effectiveness and safety of adalimumab, golimumab, and infliximab in the treatment of moderately to severely active ulcerative colitis after the failure of conventional therapies. Based on network meta-analysis, in the induction phase all 3 biologics were associated with statistically significant beneficial effects relative to placebo. Infliximab showed the greatest efficacy. (Figure 3 and 4.)
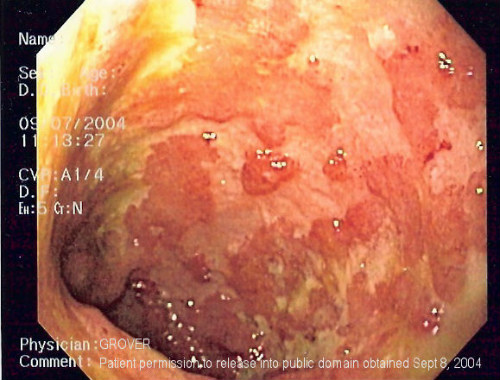
The image shows confluent superficial ulceration and loss of mucosal architecture.
(Sources: Wikipedia/Creative Commons/GNU Free.)
For patients who were found to have responded to biologic therapy at the end of the induction phase, treatment effects were not statistically significant, although the greatest effect at 8 to 32 weeks was associated with golimumab 100 mg. At 32 to52 weeks, only infliximab and golimumab 50 mg were associated with beneficial effects on clinical response.
For patients who were classified as being in remission at the end of the induction phase, all treatments except for adalimumab were associated with beneficial treatment effects versus placebo, with the greatest effect being associated with 50 mg and 100 mg of golimumab, although the effects were not statistically significant at 8–32 weeks. At 32to 52 weeks, all treatments except golimumab 50 mg were associated with beneficial treatment effects versus placebo. The greatest effect was found with being associated with adalimumab—the only treatment with statistically significant effect. Adalimumab was associated with the highest probability of persistent disease remission and the lowest probability of patients moving from remission to response and from remission to no response.

(Sources: Wikipedia/GNU Free.)
Conclusions
The reviewers concluded that that adult patients receiving one of the 3 biologics were more likely to achieve clinical response and remission than those receiving placebo. The data suggested more favorable outcomes for adalimumab and infliximab.
The biologics were, however, associated with significant safety issues that were absent in patients who received placebo or colectomy. These included serious infections, malignancies, and administration-site reactions. Nonetheless, “The economic analysis suggests that colectomy is expected to dominate drug therapies, but for some patients, colectomy may not be considered acceptable. In circumstances in which only drug options are considered, [infliximab] and [golimumab] are expected to be ruled out because of dominance, while the incremental cost-effectiveness ratio for [adalimumab] versus conventional treatment is approximately £50,300 per QALY gained,” the reviewers noted.
