- Food allergies (FA) impair quality of life in both sufferers and family.
- Allergies are associated with increased healthcare costs for sufferers, family, healthcare systems.
- Effective treatments are available to clinicians but are found to be underused.
- Food manufacturers increasingly offer alternatives to highly allergenic foods.
- Promising newer approaches are available to clinicians, such as specific oral or epicutaneous immunotherapy and the use of monoclonal antibodies.
- A good deal of research shows that early exposure to minute amounts of potential allergens can entirely prevent the development of many types of allergies.
- Evaluation of FA severity and strategies for mitigation must be part of routine primary care.
Food allergies (FA) are increasingly common both in the U.S. and throughout the world. FA place a significant financial and social burden on allergy sufferers, their family, and caregivers. Numerous strategies for preventing and treating FA are available but they appear to be underused, according to an article published recently in Clinical and Molecular Allergy.
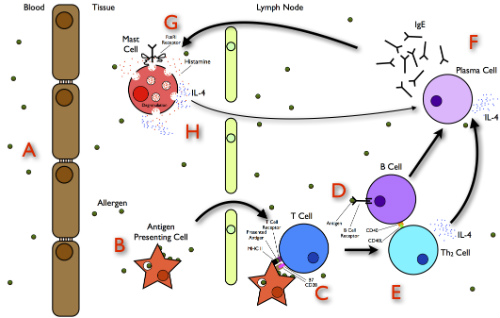
MDalert.com has published a number of articles that may be helpful for clinicians treating children at risk of acquiring FA, as well as children and adults who already suffer with these allergies. This recent article addresses strategies for prevention, as does this one from 2015. This recent article addresses both the physiologic underpinnings of allergies and proposes potential strategies for prevention and treatment. (Figure 1.)
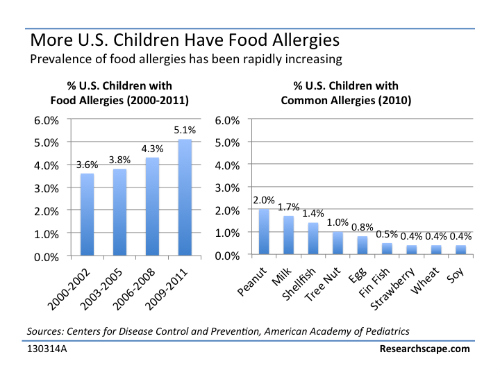
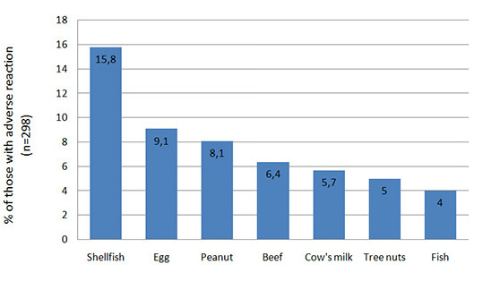
The incidence of FA, drug allergies, and environmental allergies has increased in the U.S. in other developed countries, and in developing countries. The article in Clinical and Molecular Allergy reports that allergies can have a dramatic effect on quality of life, so as to provoke fatal reactions. FA is also found to create a significant financial burden on sufferers, family, caregivers, and the broader healthcare system. (Figures 2 and 3.)
Socioeconomic Effects
The article in Clinical and Molecular Allergy focused on the socioeconomic effects that FA exerts on affected patients. The researchers performed a thorough review of the medical literature and attempted to describe the factors that may influence the quality of life of patients with FA.
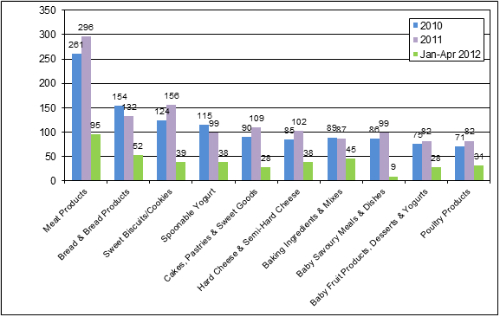
The researchers estimated the mean annual cost of healthcare for patients with FA in international dollars (I$). The annual estimate cost for FA sufferers is I$2016 and I$1089 for controls, a difference of I$927 (95 % confidence interval I$324–I$1530). “A similar result was found for adults in each country, and for children, and interestingly, it was not sensitive to baseline demographic differences. Cost was significantly related to severity of illness in cases in 9 countries,” the researchers explained. In the U.S. food manufacturers have released an increasing number of anti-allergen foods. (Figure 4.)
The authors attributed the significantly decreased health-related quality of life (HRQL) among FA sufferers to a number of factors including:
- The constant threat of exposure;
- The need for vigilance, and;
- The expectation of adverse outcomes related to allergen exposure.
Newer Clinical Strategies
These can have a tremendously adverse effect on quality of life, the authors noted. “Several studies have analyzed the impact of food allergy on health-related quality of life in adults and children in different countries. There have been described different factors that could modify HRQL in food allergic patients, the most important of them are perceived disease severity, age of the patient, peanut or soy allergy, country of origin, and having allergy to 2 or more foods,” the researchers explained.
In recent years, several different specific quality-of-life questionnaires have been devised for patients with FA. These have been developed and translated into a variety of languages and made applicable to a wide variety of cultures. These authors stressed the importance of using these questionnaires by clinicians in order to evaluate FA severity specific regions and countries, each with unique socioeconomic reality and culture.
Tools aimed at assessing the effect of FA on HRQL “should be always part of the diagnostic work up, in order to provide a complete basal assessment, to highlight target of intervention, as well as to evaluate the effectiveness of interventions designed to cure food allergy,” the authors argued. “HRQL may be the only meaningful outcome measure available for food allergy measuring this continuous burden,” they added.
To date, the primary medical strategies for managing FA include strict avoidance of the allergen food(s) and the use of emergency medications to manage allergic reactions, should they occur. The authors note, however, that additional promising approaches are available. These include the use of specific oral or epicutaneous immunotherapies, as well as the use of monoclonal antibodies. These promising strategies are progressively being investigated worldwide. However, even as an increasing number of medical centers implement the new approaches, they are not implemented widely enough in clinical practice.
