- If baseline systolic blood pressure was <140mmHg, antihypertensive treatment increased the risk of cardiovascular mortality.
- Similarly, treatment of borderline hypertension was associated with a tendency towards increased risk of all-cause mortality.
- Treatment of hypertension >150mmHg in patients with T2DM was linked to decreased risk of all-cause mortality, cardiovascular mortality, myocardial infarction, stroke, and end stage renal disease.
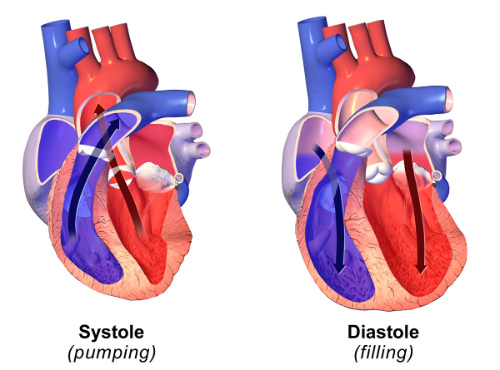
For many years, guidelines have recommended treating patients to achieve a systolic blood pressure (SBP) <130/80mmHg. Systematic reviews have questioned the evidence for these recommendations. The authors of this review endeavored to examine whether maintaining SBP <140mmHg would be beneficial in patients with T2DM. (Figure 1.)
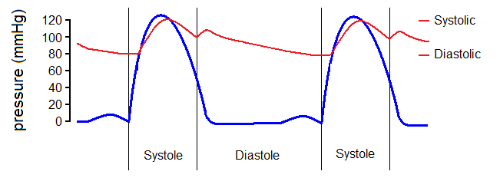
As a result of this analysis they found that antihypertensive treatment does indeed reduce the risk of mortality and cardiovascular morbidity in people with type 2 diabetes mellitus (T2DM) who have a systolic blood pressure >140mmHg. However, if SBP is <140 mm Hg antihypertensive treatment was found to be associated with an increased risk of cardiovascular death. No benefit was found that could be attributed to further decreased blood pressure.
Treating blood pressure (BP) in patients with T2DM whose SBP is already <140mmHg is linked with adverse cardiovascular outcomes, according to the results of a systematic review and meta-analysis published recently in the British Journal of Medicine. (Figure 2.)
The Analysis
The authors of this study conducted a systematic review and meta-analyses of randomized controlled trials (RCTs) in order to examine the effects on mortality and cardiovascular morbidity of antihypertensive treatment in T2DM patients with different baseline BP levels.
The reviewers included 49 RCTs (n=73,738) in the meta-analyses. Selected RCTs all included ≥100 people with T2DM who were treated for ≥12 months. All RCTs compared any antihypertensive agent against placebo, two agents against one, or different blood pressure targets.
Results
The reviewers reported that the majority of the participants in the analyzed RCTs T2DM. As would be expected, if baseline systolic blood pressure was >150mmHg, antihypertensive treatment reduced the risk of all-cause mortality (relative risk 0.89, 95% confidence interval 0.80 to 0.99), cardiovascular mortality (0.75, 0.57 to 0.99), myocardial infarction (0.74, 0.63 to 0.87), stroke (0.77, 0.65 to 0.91), and end stage renal disease (0.82, 0.71 to 0.94).
Similarly, if baseline SBP was between 140mmHg and 150mmHg, additional treatment reduced the risk of all-cause mortality (0.87, 0.78 to 0.98), myocardial infarction (0.84, 0.76 to 0.93), and heart failure (0.80, 0.66 to 0.97).
Curiously, however, if the baseline SBP was <140mmHg, further treatment increased the risk of cardiovascular mortality (1.15, 1.00 to 1.32), with a tendency towards an increased risk of all-cause mortality (1.05, 0.95 to 1.16).
Metaregression analyses showed a worse treatment effect with lower baseline SBPs for cardiovascular mortality (1.15, 1.03 to 1.29 for each 10mmHg lower SBP) and myocardial infarction (1.12, 1.03 to 1.22 for each 10mmHg lower SBP). Patterns were similar for attained SBP.
Conclusions
According to this analysis, antihypertensive treatment reduced the risk of mortality and cardiovascular morbidity in patients with T2DM and an SBP >140mmHg. If SBP was <140mmHg, however, further treatment was associated with an increased risk of cardiovascular death. Additionally, there were no observed benefits to treating hypertension in this group of patients.
