Over the last few years, the standard therapy for patients with chronic lymphocytic leukemia (CLL) has steadily shifted from monotherapy to chlorambucil to newer combinations. For CLL patients with mutated immunoglobulin heavy-chain variable region (IGHV), the current standard of care combines fludarabine, cyclophosphamide and rituximab (FCR).
Researchers recently performed a meta-analysis of five randomized controlled trials to quantify the benefit of the FCR combination for these patients, with strong results endorsing its value over other common combinations, including those using newer targeted therapies.
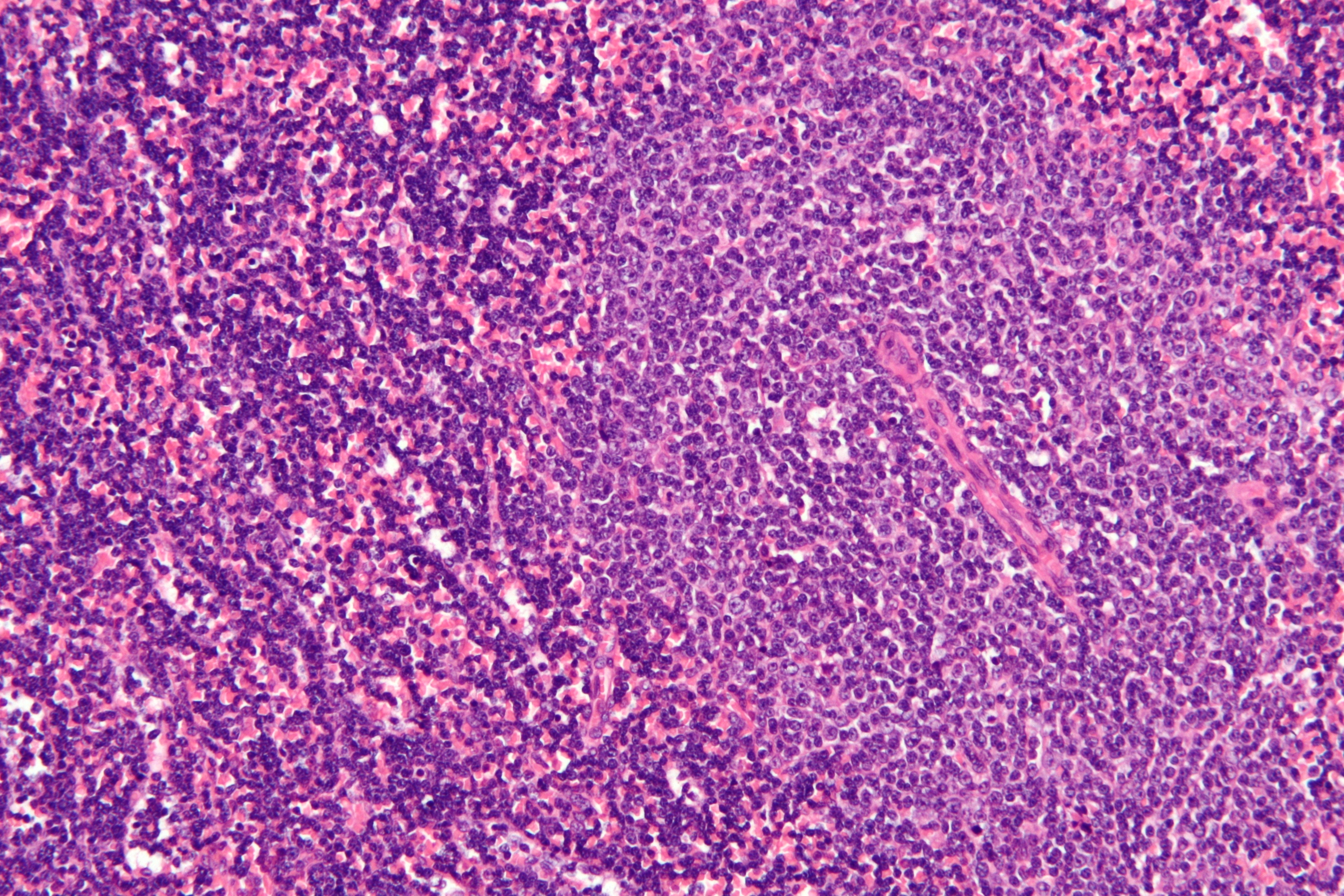
Chronic lymphocytic leukemia. (Source: Creative Commons)
Jennifer R. Brown, MD, PhD, assistant professor of medicine at Harvard Medical School and director of the Center for Chronic Lymphocytic Leukemia at the Dana-Farber Cancer Institute in Boston, and Chatree Chai-Adisaksopha, a PhD student at McMaster University in Hamilton, Ontario, found that the FCR combination improved complete remission rates as well as both progression free survival and overall survival compared to bendamustine-rituximab (BR) combinations and to ibrutinib.
From its earliest use, FCR has demonstrated an ability to produce high rates of complete response and long remissions, with some patients negative for minimal residual disease and able to discontinue treatment. Among all patients with CLL, treatment with FCR showed a 51% progression free survival (PFS) at six years in one early study and a median PFS of 6.4 years with overall PFS of 30.9% at more than 12 years in another study.
Responses were even better among patients with the IGHV mutation, with nearly 54% of IGHV-mutated patients still in remission at 12.8 years compared to just 8.7% of those without the mutation. Another study found that 71% of patients with the mutation and without other higher risk deletions remained progression free at four years—with a life expectancy similar to their age- and sex-matched peers without CLL.
The meta-analysis identified no significant difference between the overall response rate achieved by FCR and the pooled response to the five different comparators in the referenced studies, but it did demonstrate a 50% increase in the likelihood of achieving complete response with FCR regardless of IGHV mutation status.
Three studies provided minimal residual disease data and, in all three, the likelihood of achieved negative minimal residual disease was 21% higher with FCR than with the comparators: BR, fludarabine-cyclophosphamide-mitoxantrone-rituximab (FCM-R) and fludarabine, cyclophosphamide and alemtuzumab (FCCam).
Progression was 65% more likely for patients treated with comparators than those who received FCR and overall survival was 40% better for FCR than the pooled comparators.
The researchers concluded that in “fit CLL patients, FCR is the most effective chemoimmunotherapy regimen. BR is widely used but has not demonstrated the durability of remission seen with FCR and should not be considered an equivalent substitute for FCR in CLL.”
They added that FCR is not suitable for patients with renal dysfunction and certain other comorbid medical conditions and other, less intensive options should be selected for them.
