- Family physician’s contraceptive suggestions for patients were frequently not evidence based.
- The results suggested that that 23% of providers’ oral contraceptive pill recommendations and 40% of intrauterine device recommendations were inconsistent with CDC guidelines.
- As many as 50% of pregnancies are unplanned. Optimal use of contraceptive methods would reduce this number
- Results were derived from a survey study with 1054 participants.
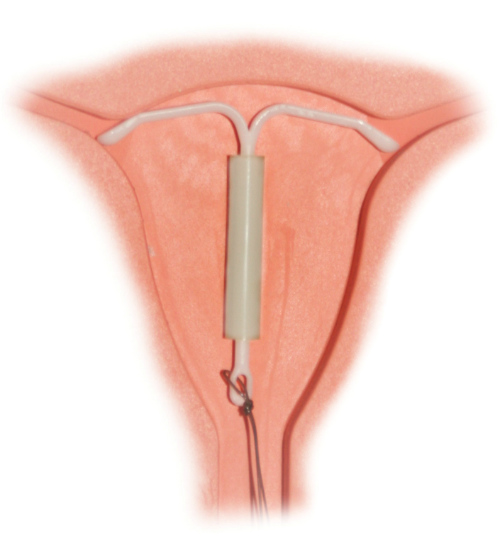
- Misconceptions were noted with regard to eligibility for use of an intrauterine device.
A study of more than 1000 family physicians suggests that a large portion of their contraceptive suggestions for patients are not evidence based. Recommendations of suboptimal or ineffective contraceptive methods may put patients at risk for unplanned pregnancies, according to a study published recently in Family Medicine. As many as 50% of pregnancies in the U.S. are unplanned. The study was conducted by members of the Department of Family Medicine at the University of Michigan in Ann Arbor.
“The contraceptive recommendations of this cohort of family medicine educators only partially reflected evidence-based guidelines. More misconceptions were noted regarding eligibility criteria for the IUD [intrauterine device] than for OCPs [oral contraceptive pills; Figure 1]. To avoid denying safe and effective contraception to otherwise appropriate candidates and putting women at risk of unintended pregnancy, evidence-based contraceptive recommendations must be improved among family medicine educators,” the authors wrote in their conclusions.
(Sources: Wikipedia/Wellcome Images/Creative Commons [CC BY 4.0]/Wikimedia Commons.)
The researchers noted that “the IUD [Figure 2] is one of the most highly effective reversible methods, yet physician misconceptions contribute to its underutilization.”
Among the 1,054 respondents (33% response rate), 98% prescribe were found to prescribe OCPs and 66% reported the use of IUDs. The OCP scale mean was 4.6 ± SD 1.6 (range 0–6), and the IUD scale mean was 4.8 SD ± 2.3 (range 0–8). These scores reflect that 23% of providers’ OCP recommendations and 40% of their IUD recommendations were inconsistent with CDC guidelines.
The Analysis
The researchers obtained survey items as part of the 2014 Council of Academic Family Medicine Educational Research Alliance (CERA) omnibus survey. This survey is distributed annually to a national cohort of U.S. family medicine educators.
The authors of the Family Medicine study created 2 summary scales designed to reflect clinical scenarios in order to assess the extent to which provider recommendations regarding eligibility criteria for oral contraceptive pills (OCPs, 6 scenarios) and the intrauterine device (IUD, eight scenarios) were consistent with guidelines issued by the Centers for Disease Control and Prevention (CDC).
The authors contributed 22 questions related to contraception to the CERA survey. They assessed contraceptive recommendations by asking respondents they prescribe any short-acting, hormonal methods such as OCPs, the progestin shot, the transdermal patch, the vaginal ring, or emergency contraceptive pills.
(Sources: Wikipedia/Creative Commons/By Hic et nunc (Own work) [Public domain], via Wikimedia Commons.)
In order to assess physician’s recommendations for the use of long-acting reversible contraceptive methods, the researchers asked providers to indicate which one of the statements best described what they would do if a patient requested an IUD or an implant:
- “I would perform the insertion myself.”
- “I would refer the woman to a colleague in my practice.”
- “I would refer the woman to an outside provider (eg, OB-GYN).”
- “I am not comfortable recommending this method at all.”
In order to assess provider’s ideas about patient eligibility for oral and hormonal contraceptive methods, the researchers focused their attention on two central issues:
- OCPs are the most commonly used reversible method among US women.
- The IUD is one of the most highly effective reversible methods, yet physician misconceptions contribute to its underutilization.
In order to tease out misconceptions about the safety and efficacy of IUDs, the researchers used 8 hypothetical scenarios in which it would be appropriate to consider the pros and cons of this contraceptive method:
- Is the woman <20 years old?
- Has she never been pregnant?
- Has she had a sexually transmitted infection (STI) within the past year?
- Has she had pelvic inflammatory disease (PID) within the past year?
- Is she taking medications for hypertension?
- Does she currently have an abnormal pap smear?
- Does she have a history of ectopic pregnancy?
- Does she have HIV infection?
Each of these scenarios represent women who are eligible for an IUD yet physicians reported making recommendations that were not evidence-based or guideline based. The researchers found that 60% of the IUD recommendations were consistent with CDC guidelines and that 40% were inconsistent with CDC guidelines.
“The percentage of respondents who would not recommend an IUD in a given situation ranged from 4.1% (for a woman taking medications for hypertension) to 46.1% (for a woman with PID 1 year ago). The rescaled median for the IUD scale was significantly lower than that for the OCP scale (3.8 and 5.0 respectively, P<.01, results not shown),” the authors explained.
