- Surgery proved to be one of the most effective treatments for spinal stenosis, according to a Cochrane meta-analysis.
- There is no greater likelihood that a patient would receive relieve from an epidural steroid injection as that he or she would from no injection at all.
- Steroid injections of various types are widely used and rarely effective.
- Rehabilitation is essential to positive outcomes.
Lumbar spinal stenosis may one of the most widespread identifiable causes of low back and leg pain among Americans. However, recent research shows that a surgical solution can be effective, as can steroid injections, local anesthetic nerve blocks, intra-articular and peri-articular injections. Accurate patient assessment, diagnosis, and rehabilitation are crucial to an optimal outcome. See our brief review of the current literature on the topic here.
What is It?
Lumbar spinal stenosis is a condition in which the spinal cord canal or spinal nerve canal narrows and compresses the spinal cord. This can lead to impaired motor and sensory conduction along the spinal cord, beginning at the point of stenosis.
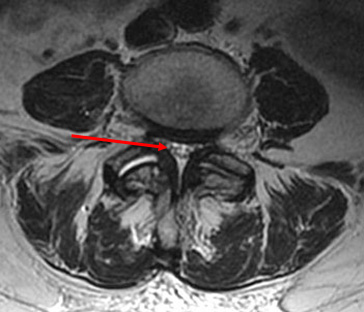
canal while the similar view on right shows a severely narrowed
or stenotic spinal canal.
The good news is that a wide variety of treatments are available and they are not infrequently curative. In long-term chronic cases, pain can often be managed without opioids.
Treatments
A number of treatments have been trialed and studied to relieve patients of pain related to spinal stenosis.
Somewhat surprisingly, surgery proved to be one of the most effective treatment for spinal stenosis. A meta-analysis found that spinal decompression was among the more effective treatments.
Transforaminal Lumbar Endoscopic Surgery
The purpose of this study was to a describe the appropriate surgical indications for transforaminal decompression performed endoscopically with the outside-in technique. The technique included foraminoplasty in patients with lateral stenosis with and without herniated disc.
These reviewers examined the records of 220 consecutive patients who had undergone percutaneous endoscopic transforaminal foraminoplasty and microdiscectomy at 228 levels. The study was conducted in order to identify the appropriate surgical indications in patients with monoradiculopathy.
At a mean of 46 months’ follow up (range 26 to 54 months), according to the Macnab criteria, excellent and good results were found for monoradiculopathy in 85% (186/220) of patients. The mean VAS score decreased from 7.5 ± 1.5 preoperatively to 2.8 ± 1.9 at the final follow-up (P<0.01). There were no approach-related complications. Clinical failures occurred in patients with bony stenoses in the lateral recess and entry zone of the neuroforamen. Less favorable outcomes were observed in patients with concomitant contained disc herniations when compared to extruded disc herniations (P<0.03) as well in patients aged older than 50 years (P<0.021).
Percutaneous, endoscopic decompression using outside-in technique works well in patients with monoradiculopathy due to lateral stenosis in the mid and exit zone of the neuroforamen. Decompression in the entry zone maybe inadequate using the transforaminal outside-in approach. Future studies with greater statistical power should determine as to whether pain relief was achieved via microdiscectomy or foraminoplasty.
Surgical Decompression
Surgical decompression of the stenosed nerve is another effective surgical approach. A multicenter Swiss study, examined the technique in 37 patients aged 80 years or older.
The objective of the study was to examine whether outcome and quality of life might improve after decompression surgery for degenerative lumbar spinal stenosis in patients older than 80 years, and to compare those data with a younger patient population from the same center.
Of the 37 patients included in the study, all showed significant improvements at 6-month and 12-month follow-ups (P<0.001). A minimal clinically important improvement was achieved with improvement of 70% in the older patient population.
“Patients 80 years or older can expect a clinically meaningful improvement after lumbar decompression for symptomatic DLSS,” the authors concluded. “Our patient population showed significant positive development in quality of life in the short- and long-term follow-ups.”
Evidence on spinal steroid injections is highly equivocal.
According to two recent studies, there is no greater likelihood that a patient would receive relieve from a steroid injection as that he or she would from no injection at all. However, in the latter case, any potential adverse events related to lumbar injections would be avoided.
A recent systematic review and meta-analysis. The researchers included 10 studies with 1,010 participants and found minimal evidence that epidural steroid injections are better than lidocaine alone. However, regardless of the mode of epidural injection, patients received mixed results following treatment of spinal stenosis with local anesthetic and steroids. However, they can concluded that “epidural steroid injections provide limited improvement in short-term and long-term benefits in [lumbar spinal stenosis patients.”
Rehabilitation
A 2013 Cochrane Database systematic review of active rehabilitation following surgery for lumbar spinal stenosis returned 1,726 results. Three of the studies were included in the final analysis (N=373). All studies were deemed to have low risk of bias and no study had unacceptably high dropout rates; typical of Cochrane meta-analyses.
The reviewed evidence appears to suggest that active rehabilitation is more effective than usual care in improving both short- and long-term (back-related) functional status. Similar findings were noted for secondary outcomes, including short-term improvement in low back pain and long-term improvement in both low back pain and leg pain, although limited impact was observed in relation to improvements in general health status. The clinical relevance of these effects is medium to small. Our evaluation is limited by the small number of relevant studies identified, and further research is required.
