- Learn more about AMA PCPI, CMS PQRS, HEDIS, and the specific measures that apply to your specialty and position.
- The AMA has created more than 350 individual measures in 47 subject areas.
- The CMS has implemented myriad new PQRS measures.
- The Joint Commission, the NCQA, and the HEDIS measures are also frequently used to evaluate physicians and practices.
- Opportunity remains for healthcare institutions of all sizes to create their own performance metrics. Guidance on this process is widely available.
- Payors want improved outcomes at lower cost, and their willing to pay docs additionally to achieve this.
Performance and Measurement
Efforts are underway throughout the United States, by the Centers for Medicare and Medicaid Services (CMS) and other national agencies, and regionally by many hospital systems, hospitals, small practices, and by private payors, to develop reporting and payment systems that support and reward quality and the efficient delivery of care.
The American Medical Association (AMA) offers the following metrics based on its own Physician Consortium for Performance Improvement (PCPI). According to the AMA website the PCPI and PCPI-approved quality measures include:
- Measurement sets in 47 clinical areas and preventive care
- More than 350 individual measures
- Clinically relevant means for tracking variations in care
- Guidance and methods that have advanced the science of measure development
The metrics that matter continue to evolve. Physicians can research the specific AMA PCPI metrics here. The CMS offers significant resources here. The CMS list of measures is available here. The CMS PQRS implementation guide is available here.
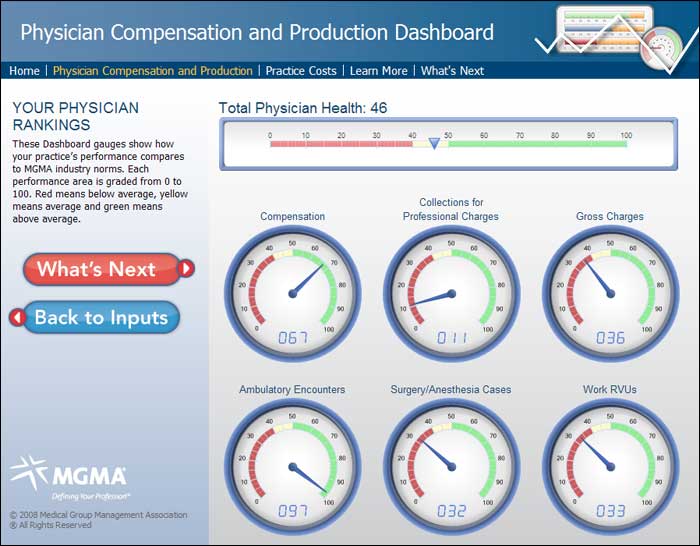
The website Dashboard Spy offers tools for creating compliance dashboards such as the one in Figure 1. This one is licensed to the Medical Group Management Association.
Compensation and Employment
Compensation and employment models for physicians now include a number of measures. Over the past 25 years, these measures of performance quality have been promulgated by a variety of regulatory bodies including the Joint Commission, the National Committee for Quality Assurance (NCQA), and the Healthcare Effectiveness Data and Information Set (HEDIS).
The most notable focus on individual physician measurement of care quality has been the implementation by CMS of the Physician Quality Reporting Initiative (PQRI) in 2006 and the the Physician Quality Reporting System (PQRS) currently in effect.
Financial disincentives for failure to report PQRS data to CMS beginning in 2015 have compelled physician practices to develop and implement systems for the accurate capture and reporting of quality measures for their clinical and cost outcomes.
The Upside
Many of the new metrics are linked directly to compensation and reimbursement. Payors want improved outcomes at lower cost, and their willing to pay docs additionally to achieve this. The Healthcare Strategy Group offers the following examples:
“Although these measures are focused on patient outcomes, many organizations may choose to adapt such measures to focus on the process of care. Hemoglobin A1c control, for example, could be adapted to focus on the percentage of patients who had Hemoglobin A1c testing within the past year. NCQA benchmark data can then be used to establish the compliance percentages and percentiles that trigger the physician “passing” the quality indicator.
The quality bonus pool can also be staged (example: less than 85% patient compliance pays 0% quality bonus, 85% to 90% patient compliance triggers payment of 50% quality bonus, greater than 90% patient compliance triggers payment of 100% quality bonus),” according to the Healthcare Strategy Group website.
Under the Microscope: Specific Measures
HEDIS includes performance measures related to dozens of important healthcare issues. Examples of selected measures applicable to primary care physicians include, but are not limited to:
- Advising smokers to quit
- Antidepressant medication management
- Breast cancer screening
- Cervical cancer screening
- Children and adolescent access to primary care physician
- Children and adolescent immunization status
- Comprehensive diabetes care
- Controlling high blood pressure
- Prenatal and postpartum care
HEDIS includes many other metrics for primary care docs, and myriad others for specialists.
The Healthcare Strategy Group article offers specific examples. Two of the most common diabetes-related PQRS violations are as follows:
- Diabetes: Hemoglobin A1c Poor Control: Percentage of patients aged 18 to 75 years with diabetes who had hemoglobin A1c >9.0% during the measurement period.
- Diabetes: Low Density Lipoprotein (LDL-C) Control (<100 mg/dL): Percentage of patients aged 18 to 75 years of age with diabetes whose LDL-C was adequately controlled (<100 mg/dL) during the measurement period.
Performance Measures within an Ambulatory Surgery Center
An article in ASC Review reiterates the notion that metrics are a good thing. “You don’t know how well you are doing unless you can measure,” according to Sandy Berreth, administrator of Brainerd Lakes Surgery Center in Baxter, Minn.
Here are 9 physician performance metrics chosen by Ms. Berreth and Ann O'Neill, director of clinical operations at Regent Surgical Health in Westchester, Ill.
- On-time starts.
- Utilization of block time.
- Case volume.
- Cost of staff per case.
- Cost of supplies per case.
- Infection rates.
- Surgical complications.
- Hand-washing compliance.
- On-time completion of medical records.
Obviously, it is important for you to know the measures that are being used to gauge the quality of your performance. Whether you are subject to CMS metrics, private payor metrics, the metrics created by your own practice, or a combination thereof, take the time to learn the specifics, and to stay ahead in the measurement game.
