- Stroke kills almost 130,000 Americans each year, according to the Centers for Disease Control and Prevention (CDC).
- Intracranial hemorrhage (ICH) comprises 10% to 15% of all strokes.
- Approximately 37,000 to 53,000 people suffer an ICH annually.
- Incidence of ICH is down but related mortality remains high.
- Ambient temperature did not correlate with risk for stroke or subarachnoid hemorrhage.
- Change in temperature over the previous 24 hours appeared to be more important than absolute temperature with regard to risk of stroke or ICH.
- Lancet study finds that 90% of strokes are preventable.
Change in ambient temperature of the past 24 hours – specifically, decrease in temperature – correlates with an increased risk of intracranial hemorrhage (ICH), according to a study published recently in the International Journal of Environmental Research and Public Health. The study, “Ambient Temperature and Stroke Occurrence: A Systematic Review and Meta-Analysis,” found that that lower mean ambient temperature was significantly associated with ICH risk (Figure 1).
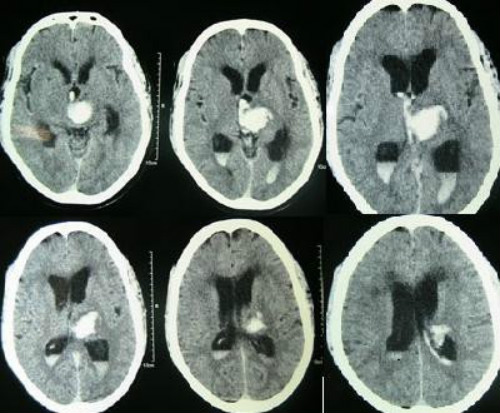
with associated hydrocephalus and blood in the third and both lateral ventricles.
(Sources: Wikipedia/By Yadav YR, Mukerji G, Shenoy R, Basoor A, Jain G, Nelson A - Yadav YR, Mukerji G, Shenoy R, Basoor A, Jain G, Nelson A (2007). "Endoscopic management of hypertensive intraventricular haemorrhage with obstructive hydrocephalus". BMC Neurol./Creative Commons.)
This meta-analysis included 21 studies and 476,511 patients. Of the 21 studies, two were community-based, 14 were population-based, and five were based on stroke registries. Seven studies were defined as high quality as they met five of the quality criteria, another seven met four and the remainer met less than four of the quality criteria. In brief, studies were conducted in 12 countries, across five continents; only two studies were conducted in the Southern Hemisphere. Seven studies were from countries with latitude less than 30 degrees and 14 were between 30 and 60 degrees.
In this comprehensive review, a consistent association of daily mean, minimum or maximum ambient temperature with IS, and SAH occurrence was not identified. In particular, conclusions were limited by the inability to pool all studies because of a lack of crude data and heterogeneity in data presentation. However, we found that lower mean ambient temperature was significantly associated with ICH risk. Subgroup analysis showed that lower temperature increased IS risk in women, and older age appeared to increase vulnerability to temperature for both IS and ICH. Furthermore, change in ambient temperature over the previous 24 h appeared to be more important, especially in relation to ICH risk.
In conclusion, available data on the evidence for an association between ambient temperature and incidence of stroke are conflicting. This review shows that lower mean ambient temperature is significantly associated with ICH risk, but not with IS and SAH. Importantly, further research is needed to clarify the extent and nature of any relationship between temperature and stroke in different geographical areas, and in respect of stroke subtype.
Background
Intracerebral hemorrhage (Figure 2) represents approximately 10% to 15% (10-30/100,000 population) of all strokes. About 2 million of the 15 million strokes worldwide are intracerebral hemorrhages. Men are more likely to suffer an intracerebral hemorrhage than women.
Each year, approximately 37,000 to 52,400 people suffer from an intracerebral hemorrhage. The number of intracerebral hemorrhages is expected to increase substantially over the next few decades as the population ages. Major underlying causes for the increasing incidence include more frequent use of anticoagulant medication and age-related brain changes, according to the website of the Minneapolis Clinic of Neurology.
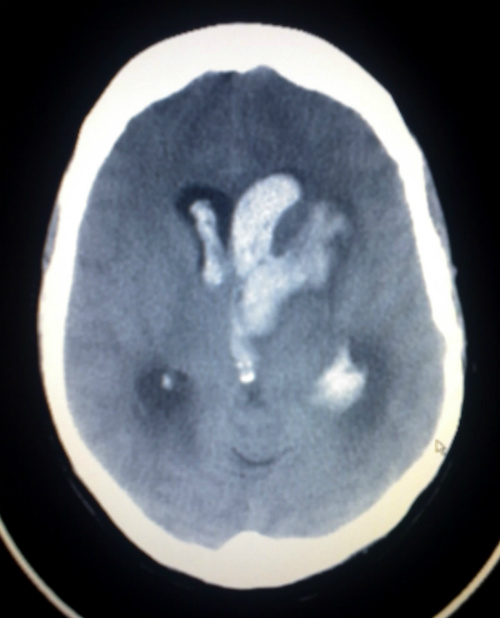
(Sources: Wikipedia/By Glitzy queen00/Public Domain.)
Estimates from the Global Burden of Diseases, Injuries, and Risk Factors Study ranked stroke as the second most common cause of death and the third most common cause of disability-adjusted life-years (DALYs) worldwide in 2010. In 2010, the absolute number of people with first stroke (16.9 million), stroke survivors (33 million), stroke-related deaths (5.9 million), and DALYs lost (102 million) were extremely high, having increased significantly since 1990 (increases of 68%, 84%, 26% and 12%, respectively), according to the authors if the study published in the International Journal of Environmental Research and Public Health.
ICH Mortality Remains High
A separate study published in Neurology in 2014 found that while the incidence of ICH is declining, related mortality remains high (Figure 3).
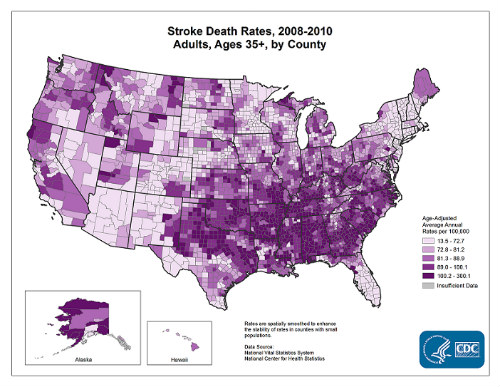
(Source: CDC/Public Domain.)
“ICH incidence decreased over the past decade, but case fatality and long-term mortality were unchanged. This suggests that primary prevention efforts may be improving over time, but more work is needed to improve ICH treatment and reduce the risk of death,” the authors concluded.
The authors of this study identified all cases of spontaneous ICH in a South Texas community during the period 2000 to 2010 using data from the Brain Attack Surveillance in Corpus Christi Project. Trends in 30-day mortality and long-term mortality were estimated with log-binomial or Cox proportional hazards models adjusted for demographics, stroke severity, and comorbid disease, the authors explained.
The authors identified 734 cases of ICH. The adjusted ICH annual incidence rate was 5.21 per 10,000 (95% confidence interval [CI] 4.36, 6.24) in 2000 and 4.30 per 10,000 (95% CI 3.21, 5.76) in 2010. The statistics demonstrate a clear reduction in the frequency of ICH among this population.
“The estimated 10-year change in demographic-adjusted ICH annual incidence rate was -31% (95% CI -47%, -11%). Yearly demographic-adjusted 30-day case fatality ranged from 28.3% (95% CI 19.9%, 40.3%) in 2006 to 46.5% (95% CI 35.5, 60.8) in 2008,” they wrote.
Vast Majority of Strokes Are Preventable
Ten potentially modifiable risk factors are collectively associated with about 90% of strokes in each major region of the world, among ethnic groups, in men and women, and in all ages, according to a study published recently in The Lancet.
In other words, “Nine out of 10 strokes are preventable, according a global study that shines light on one of the world's leading causes of death and disability,” according to a report on The Lancet study published in U.S. News and World Report.
The report in The Lancet confirms that 10 modifiable risk factors account for 90% of strokes worldwide. The Lancet study, called INTERSTROKE, examined nearly 27,000 people in 32 countries across all continents. The authors found that hypertension is the leading risk factor for stroke. Others include lack of physical activity, obesity, stress, diabetes, and poor diet.
The researchers examined strokes worldwide that occurred between Jan 2007 and Aug 2015. In all, 26 919 participants were recruited from 32 countries (13,447 cases; 10,388 with ischemic stroke, 3059 with ICH, and 13,472 controls).
Modifiable risk factors that were associated with increased risk of stork included:
- Alcohol consumption
- Cardiac causes
- Current smoking
- Diabetes mellitus
- High levels of apolipoprotein
- High waist-to-hip ratio
- History of hypertension or borderline hypertension
- Lack of regularly physical activity
- Poor diet
- Psychosocial factors
“We observed regional variations in the importance of individual risk factors, which were related to variations in the magnitude of ORs (odds ratios; rather than direction, which we observed for diet) and differences in prevalence of risk factors among regions. Hypertension was more associated with intracerebral hemorrhage than with ischemic stroke, whereas current smoking, diabetes, apolipoproteins, and cardiac causes were more associated with ischemic stroke (P<0·0001),” the Lancet authors wrote.
Put another way, for each of the 10 risk factors, there is a corresponding reduction in stroke risk if the risk factor did not exist:
- Without hypertension, stroke risk decreases by 47.9 percent
- Regular physical activity reduces stroke risk by 35.8%
- Improved diet could reduce stroke risk by 23.2%.
- Taken together, removing modifiable risk factors from the picture results in a nearly 91% reduction in stroke risk, irrespective of region studied, age range, or gender.
"Our findings will inform the development of global population-level interventions to reduce stroke, and how such programmes may be tailored to individual regions, as we did observe some regional differences in the importance of some risk factors by region. This includes better health education, more affordable healthy food, avoidance of tobacco, and more affordable medication for hypertension and dyslipidemia,” explained said Lanced study author Salim Yusuf, MD, of the Population Health Research Institute at McMaster University, in a press release.
