Topical Calcineurin Inhibitors Prescribed for Atopic Dermatitis May Increase Lymphoma Risk
By Cameron Kelsall, /alert Contributor
April 13, 2021
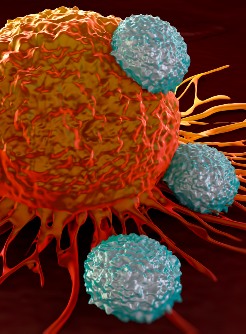
A systematic review and meta-analysis published in JAMA Dermatology identified a potential link between topical calcineurin inhibitors (TCIs) and an increased risk for lymphoma.
However, the association did not extend to other forms of cancer, and the absolute risk for lymphoma among users of TCIs remained low.
TCIs are used frequently as a second-line treatment for patients with atopic dermatitis following first-line topical corticosteroids. In 2006, the US Food and Drug Administration added a black box warning for potential increased cancer risk among patients using TCIs.
“Of the more than 6.7 million patients receiving TCI treatment, the black box warning was based on approximately 25 case reports, without systematic analysis supporting causation between TCI use and malignant neoplasms,” wrote Aaron M. Drucker, MD, ScM, FRCPC, associate professor of dermatology at University of Toronto, and colleagues. “Given the long potential latency for cancer development, postmarketing studies with long follow-up are necessary to determine whether there is an association between TCIs and cancer.”
Drucker and colleagues performed a database search to identify observational studies analyzing the relationship between TCI use and cancer diagnoses. Studies were eligible for inclusion if they evaluated the risk for cancer in patients receiving TCIs compared with an active or nonactive control group.
Overall cancer risk served as a study endpoint, as well as the specific risk for lymphoma, melanoma or keratinocyte carcinoma.
The researchers identified 11 studies meeting their inclusion criteria (cohort studies, n = 8; case–control studies, n = 3). The eight cohort studies represented 408,366 patients treated with TCIs, as well as 1,764,313 nonactive comparators and 1,067,280 participants treated with topical corticosteroids. The three case–control studies represented 3,898 participants with cancer and 14,026 cancer-free participants.
The researchers observed no association between TCI use and overall cancer risk when compared with nonactive comparators (pooled relative risk [RR], 1.03; 95% CI, 0.92-1.16; I2 = 10%). Results were similar in two studies that reported cancer risk in pediatric cohorts (pooled RR, 1.10; 95% CI, 0.59-2.06; I2 = 0%), and no studies included an analysis of the overall cancer risk of TCIs compared with topical corticosteroids.
The risk for lymphoma increased with TCI use when compared with nonactive comparators (pooled RR, 1.86; 95% CI, 1.39-2.49; I2 = 27%) and topical corticosteroids (pooled RR, 1.35; 95% CI, 1.13-1.61; I2 = 0%).
The researchers did not observe an association between TCI use and increased risk for melanoma or keratinocyte carcinoma. Results from one case–control study suggested that tacrolimus use was associated with a significantly reduced risk for keratinocyte carcinoma (odds ratio, 0.43; 95% CI, 0.3-0.6).
“Overall, our findings suggest an association between TCI use and risk of lymphoma but with no increased risk of other cancers, including skin cancers,” the researchers concluded. “Given that the absolute risk of lymphoma is low, particularly in children, the increase in relative risk translates to a very small increase in the absolute risk of lymphoma for a given patient.”












.jpg)





.jpg)





.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)