- The analysis included 30 randomized clinical trials (RCTs) and 11,964 patients.
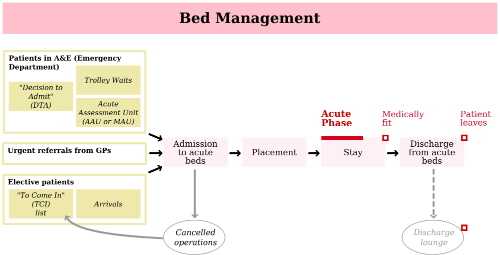
- Patient-centric discharge plans were associated with reduced readmission rates and improved satisfaction among patients and providers.
- Individualized plans were also associated with reduced length of hospital stay.
- Patients included in the trials included medical patients, surgical patients, patients with a combination of medical and surgical conditions, patients who had been injured in a fall, and patients treated in a psychiatric hospital.
- Evidence that patient-centric discharge plans reduced overall cost of care was inconclusive.
A patient-centric discharge can reduce hospital readmission rates, according to the results of a recently updated Cochrane analysis of randomized controlled trials (RCTs). An individualized discharge plan can also reduce hospital length of stay and reduce the risk of hospital readmission at 3 months for older patients a medical condition.
Such discharge planning may also result in increased satisfaction among both patients and care providers. Little evidence was found that individualized discharge planning reduces healthcare costs.
The Analysis
The Cochrane reviewers evaluated 30 RCTs including 11,964 patients. RCTs that compared an individualized discharge plan with routine discharge care were included. All participants were hospital inpatients.
“We grouped studies according to patient groups (elderly medical patients, patients recovering from surgery, and those with a mix of conditions) and by outcome,” the authors explained. “We performed our statistical analysis according to the intention-to-treat principle, calculating risk ratios (RRs) for dichotomous outcomes and mean differences (MDs) for continuous data using fixed-effect meta-analysis.”
Of the 30 RCTs evaluated, 21 included older participants with a medical condition, 5 included patients with a mix of medical and surgical conditions, 1 trial included patients from a psychiatric hospital, 1 from both a psychiatric hospital and a general hospital, and 2 trials recruited participants admitted to hospital following a fall.
Hospital length of stay and readmissions to hospital were reduced for participants admitted to hospital with a medical diagnosis and who were allocated to discharge planning (length of stay MD was -0.73, 95% confidence interval [CI] -1.33 to - 0.12, 12 trials, moderate certainty evidence; readmission rates (RR) 0.87, 95% CI 0.79 to 0.97, 15 trials, moderate certainty evidence).
The authors noted that “It is uncertain whether discharge planning reduces readmission rates for patients admitted to hospital following a fall (RR 1.36, 95% CI 0.46 to 4.01, 2 trials, very low certainty evidence). For elderly patients with a medical condition, there was little or no difference between groups for mortality (RR 0.99, 95% CI 0.79 to 1.24, moderate certainty). Similarly, there was also little evidence regarding mortality for participants recovering from surgery or who had a mix of medical and surgical conditions.
Discharge planning appeared to be linked to increased satisfaction for patients and healthcare professionals (low certainty evidence, 6 trials). It was unclear whether there is any difference in the cost of care when discharge planning is implemented with patients who have a medical condition. A discharge plan tailored to the individual patient was linked to reduced hospital length of stay and reduced risk of readmission 3 months for older people with a medical condition.
