- Smoking cessation programs are highly cost-effective; The economic cost and healthcare expenditure associated with tobacco use are estimated at $97 billion and $96 billion, respectively.
- Results support the long-term (≥12 months) efficacy of preoperative smoking cessation programs.
- Five million deaths are attributed to tobacco annually in the U.S, annual mortality will increase to 8 million by 2030.
- Projections suggest that tobacco will kill more people than any single disease pathology by 2020.
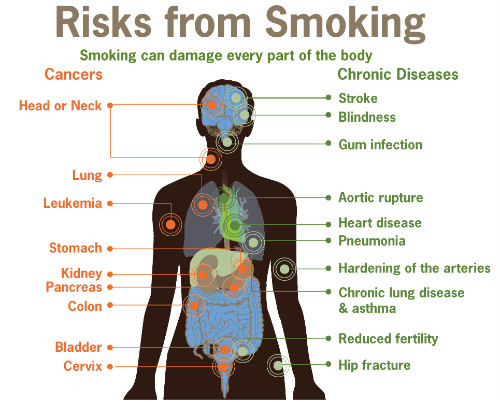
Tobacco use is the leading cause of preventable death both in the U.S and worldwide. Each year tobacco use leads to the deaths of 5 million people. The authors of a systematic review and meta-analysis suggest that by 2020, tobacco will kill more people than any single disease pathology. Annual tobacco-related mortality could increase to 8 million people by 2030. Tobacco smokers die on average 10 years earlier than their nonsmoking counterparts.
Background
According the results of a meta-analysis and systematic review published recently in the American Journal of Managed Care (2015;21(11):e623-e631) pre-operative smoking cessation programs can lead to long-term abstinence in a highly cost-effective manner.
Diseases associated with tobacco use include cancers, cardiovascular disease, respiratory disease, both ischemic and embolic events, among others. In the United States alone, the economic cost and healthcare expenditure associated with tobacco use is estimated at $97 billion and $96 billion, respectively, according to the report.
With a dual focus on cost containment and improved clinical outcomes, reduction in rates of tobacco are a prime target for intervention. In the primary care setting, patients present to their primary care physician with multiple complaints, many of which are tobacco related. Many primary care physicians are frustrated in their attempts to help patients reduce or eliminate tobacco use. Therefore, perioperative care presents a unique opportunity to help patients quit using tobacco.
The authors of this review suggest that that approximately 10 million tobacco smokers undergo surgery each year in the U.S. “Moreover, surgery precipitates spontaneous uptake of risk-reducing health behaviors—it is a documented “teachable moment” for smoking cessation,” the authors wrote.
Studies suggest that preoperative smoking cessation interventions can increase postoperative abstinence by up to 60%, with each additional week of cessation producing an improved cumulative effect. Surgeons, anesthesiologists, nurses, and other presurgical staff can exploit this opportunity, to both improve surgical outcomes and to promote smoking cessation.

Interventions
Smoking cessation interventions studied began at a minimum of 3 to 7 days before surgery. The maximum began 6 months preoperatively. In most cases the programs emphasized self-efficacy. However, 4 of the reviewed studies employed a nurse-driven approach; 1 study used an interactive computerized smoking cessation program.20
In every study but 1, a face-to-face method of contact during the intervention was used; 3 studies also included. Nicotine replacement therapy (NRT) was offered free of charge in 4 studies and was highly encouraged in 1 quasi-experimental study. However, just 2 studies reported the timing or length of the NRT. In 1 study patients were given nicotine replacement 6 to 8 weeks before surgery. In the other study patients were given NRT 2 days before surgery until 10 days postop.
The verification method for smoking cessation at 6, 9, and 12 months postoperatively varied among the studies. In 3 studies either expired carbon monoxide or presence of urine cotinine was used. In 5 studies the researchers relied on self-reporting of smoking cessation behavior.
The Analysis
The authors of this review examined randomized controlled trials (RCTs) and quasi-experimental studies in order evaluate the association between preoperative smoking cessation programs and long-term smoking cessation at ≥6 months postop.
The analysis included 4 RCTs and 4 quasi-experimental studies. Two RCTs demonstrated an association between interventions and cessation at 12 months, and the quasi-experimental studies showed cessation rates of 48% to 56% at 12 months after surgery. Interventions were associated with a greater likelihood of cessation at 12 months (P=0.02).
Conclusion
The literature suggests that preoperative smoking cessation programs frequently lead to long-term cessation of ≥12 months’ duration, the authors concluded.
