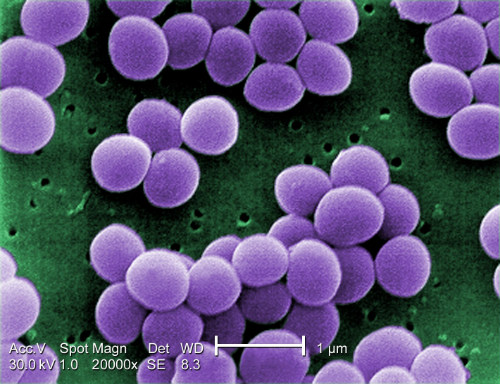
- Health care-associated infection outbreaks have occurred in outpatient settings due to lapses in infection-prevention protocols
- Cross-sectional survey published in the American Journal of Infection Control used medical student observers of infection prevention, hand hygiene, and injection safety in outpatient settings.
- Of the 163 injection safety observations, only 66% of the preparations complied with all of the recommended infection-prevention steps.
- Outpatients are a considerable risk of infection transmission do to these lapses which are easily avoided by following established protocols.
Proper hand-hygiene protocols were not followed in an alarming number of outpatient encounters according to a cross-sectional survey study published recently in the American Journal of Infection Control (AJIC). The study evaluated the rate of proper hand-hygiene practices at 15 outpatient sites in New Mexico in 2014 (Figure 1). Medical practice staff interviews reported a mean of 92.8% (median, 96.7%; range, 75.0%-98.9%) presence of recommended policies and practices. However, independent observers reported that hygiene protocols were followed in little more than 60% of outpatient encounters.

This research project “highlights the importance of assessing both the report of recommended infection prevention policies and practices as well as behavior compliance through observational audits. The project findings identify areas for public health patient safety policy and prevention efforts (Figure 2). In addition, this project provided an opportunity to build an area of significant public health and medical practice collaboration, beyond the traditional relationship, which is critical for health care provider education and continuing education. Future work may include assessments to better understand barriers to infection prevention compliance, such as for hand hygiene and injection safety, and the ability of systems solutions to improve compliance,” the authors explained.

The researchers used a cross-sectional study design to assess infection prevention policies and practices during a medical student outpatient rotation. The healthcare providers (HCPs) completed a standardized infection prevention checklist was completed following each encounter. Observations of proper injection safety practices and hand hygiene behavior were conducted by medical student observers.
The observers tracked 163 injection safety observations that revealed medication vial rubber septums were disinfected with alcohol before piercing in 78.4% of cases (95% confidence interval [CI], 71.1%-84.7%). The observations of 333 hand-hygiene instances revealed 33.9% (95% CI, 28.8%-39.1%) use of alcohol-based hand rub lotions, 29.1% (95% CI, 24.2%-34.0%) use of soap and water, and 37.0% (95% CI, 31.8%-42.4%) use of no hand hygiene, according to the ACIJ report. (Figure 3.)
“These findings support the need for ongoing infection prevention quality improvement initiatives (Figure 4) in outpatient settings and underscore the importance of assessing both self-report and observed behavior of infection prevention compliance,” the authors explained
According to these researchers, the lack of hand-hygiene compliance is not explained by lack of available supplies or education. All the healthcare settings observed reported and were observed to have adequate hygiene supplies. A high percentage of the HCPs at these sites reported that they had received hand-hygiene education. “However, despite knowledge of hand hygiene importance, there can be both real and perceived barriers to hand hygiene that need to be addressed to improve compliance,” the researchers explained.

Among the barriers to proper adherence infection control protocols, the researchers noted the following:
- Inappropriate or non-ergonomic location can pose barriers to hand hygiene;
- Concerns about skin irritation;
- Interference with worker–patient relationship;
- Wearing gloves;
- High workload, and;
- Under staffing.
“Systems and design solutions can help reduce some barriers, such as locating alcohol handrub dispensers inside and outside of every exam room door, so that hand hygiene performance is convenient and easy to perform. Availability of alcohol handrub, which tends to be less irritating than soap and water, as well as availability of free skin-care lotion may help alleviate barriers related to skin irritation. Understanding and quantifying health care provider preferences for hand hygiene method could be useful in promoting adherence to hand hygiene and in ensuring that supplies for hand hygiene are readily available and placed appropriately and conveniently,” the authors concluded.
