- Three cases of sexually transmitted Zika virus are reported in Texas.
- “Sexual transmission of Zika virus is possible, and is of particular concern during pregnancy,” CDC.
- Men who reside in or have traveled to an area where Zika virus transmission is active and who have a pregnant partner should abstain from sexual activity or consistently use condoms during sex.
- The virus appears to be contained in semen and has been transmitted by men who later developed symptomatic illness. The duration of persistence of Zika virus in semen remains unknown.
- Centers for Disease Control and Prevention (CDC) recommends the use of condoms during all forms of sexual contact between partners who have traveled to or reside in Zika-infected areas.
The U.S. Centers for Disease Control and Prevention (CDC) has recommended the use of condoms during all forms of sexual contact between partners following the man’s travel to Zika-infected areas. There have been 35 cases of travel-associated Zika in the U.S. and 9 locally transmitted cases, according to a CDC interim report issued on February 5, 2016. “Sexual transmission of Zika virus is possible, and is of particular concern during pregnancy,” according to the CDC report.
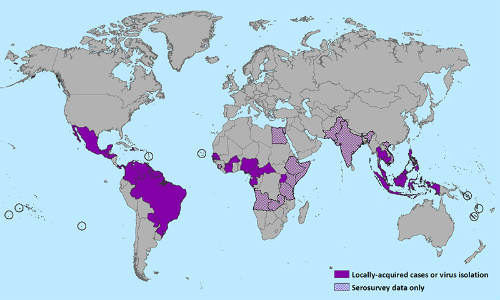
As reported recently on MDalert.com, the Zika virus appears to be spreading north from highly-infected areas including Brazil (estimated 1.5 million cases), Columbia (estimated 20000 cases), Honduras (3649 cases), Venezuela (3700 cases), El Salvador (estimated 2500 cases), Haiti (125 cases), Puerto Rico (22 cases), and others. (Figure 1.) The vast majority of these cases have been identified in 2016.
The CDC recommends testing for Zika virus in pregnant women. However, Zika virus testing for the assessment of risk for sexual transmission is of uncertain value, because current understanding of the incidence and duration of shedding in the male genitourinary tract is limited to the 1 case report in which Zika virus persisted longer in semen than in blood. At this time, testing of men for the purpose of assessing risk for sexual transmission is not recommended, the CDC report notes.
CDC Recommendations for Sexual Contact Between Men and Their Pregnant Partners
Men who reside in or have traveled to an area where Zika virus transmission is active and who have a pregnant partner should abstain from sexual activity or consistently use condoms during sex (ie, vaginal intercourse, anal intercourse, or fellatio) for the duration of the pregnancy. Pregnant women should discuss their male partner’s potential exposures to mosquitoes and history of Zika-like illness with their healthcare provider. Healthcare providers can consult the CDC guidelines for evaluation and testing of pregnant women.
The CDC recommendations for men who reside in or have traveled to areas with active Zika virus transmission and their sex partners (Available here.) The recommendations will be revised as information becomes available.
The Zika Virus and Zika Fever
Zika virus is a mosquito-borne flavivirus primarily transmitted by Aedes aegypti mosquitoes (Figure 2). Infection with Zika virus is asymptomatic in approximately 80% of cases, according to the CDC. When the virus does cause illness, symptoms are generally mild and self-limited.

However, recent evidence suggests a link between maternal Zika virus infection and adverse fetal outcomes, including microcephaly and potential association with Guillain-Barré syndrome. There are currently no effective strategies for treatment of Zika infection. No vaccine has yet been formulated. The only strategies for prevention include taking steps to prevent mosquito bites, such as covering exposed skin and the use of insect repellents formulated with DEET.
Sexual Transmission of the Zika Virus
Current information about possible sexual transmission of Zika is based on 3 reports. The first was probable sexual transmission of Zika virus from a man to a woman in which sexual contact occurred a few days before the man’s symptom onset, according the CDC report. The second case is still under investigation by the Dallas County Department of Health and Human Services in Texas. The third case is a single report of Zika virus isolated from semen ≥2 weeks to as many as 10 weeks following the onset of illness.
Reverse transcriptase-polymerase chain reaction testing of blood plasma specimens collected at the same time as the semen specimens did not detect Zika virus, the CDC report explained. The man had no sexual contacts. Because no further testing was conducted, the duration of persistence of Zika virus in semen remains unknown.
In all 3 cases, the men developed symptomatic illness. Whether infected men who never develop symptoms can transmit Zika virus to their sex partners is unknown. Sexual transmission of Zika virus from infected women to their sex partners has not been reported. Sexual transmission of many infections, including those caused by other viruses, is reduced by consistent and correct use of latex condoms (Figure 3), the CDC report explains.

in order to prevent the sexual transmission of the Zika virus.
CDC Recommendations for Men and Their Non-Pregnant Sex Partners
Men who reside in or have traveled to an area of active Zika virus transmission should either abstain from sexual activity or consistently use condoms during all forms of sexual contact. Most infections are asymptomatic, and when illness does occur, it is usually produces mild symptoms lasting from several days to a week. Severe disease requiring hospitalization is uncommon. The risk for acquiring mosquito-borne Zika virus in areas of active transmission depends on the duration and extent of exposure to infected mosquitoes and the steps taken to prevent mosquito bites. After infection, Zika virus might persist in semen after it is no longer detectable in blood.
