- Paravertebral blockade was associated with fewer short-term complications compared to thoracic epidural blockade for thoracotomy.
- Reduced pain was presumably associated with higher patient satisfaction.
- Reduced short-term complications were presumably associated with reduce short-term hospital costs.
- No differences were found in 30-day mortality, major complications, or length of hospital stay.
- The reviewers found insufficient data on chronic pain and costs.
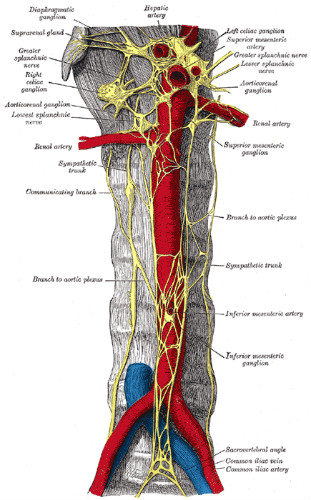
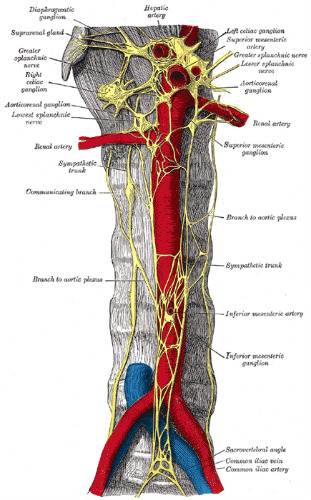
Paravertebral blockade (PVB) (Figure 1) was associated with fewer short-term complications compared to thoracic epidural blockade (TEB) (Figure 2) for thoracotomy, according to a recent Cochrane systematic review and meta-analysis. Paravertebral blockade was equally as effective as thoracic epidural blockade in controlling acute pain.
The analysis did not reveal reliable data on other outcomes. For instance, the reviewers found no differences in 30-day mortality, major complications, or length of hospital stay. There was insufficient data on chronic pain and costs.
Background
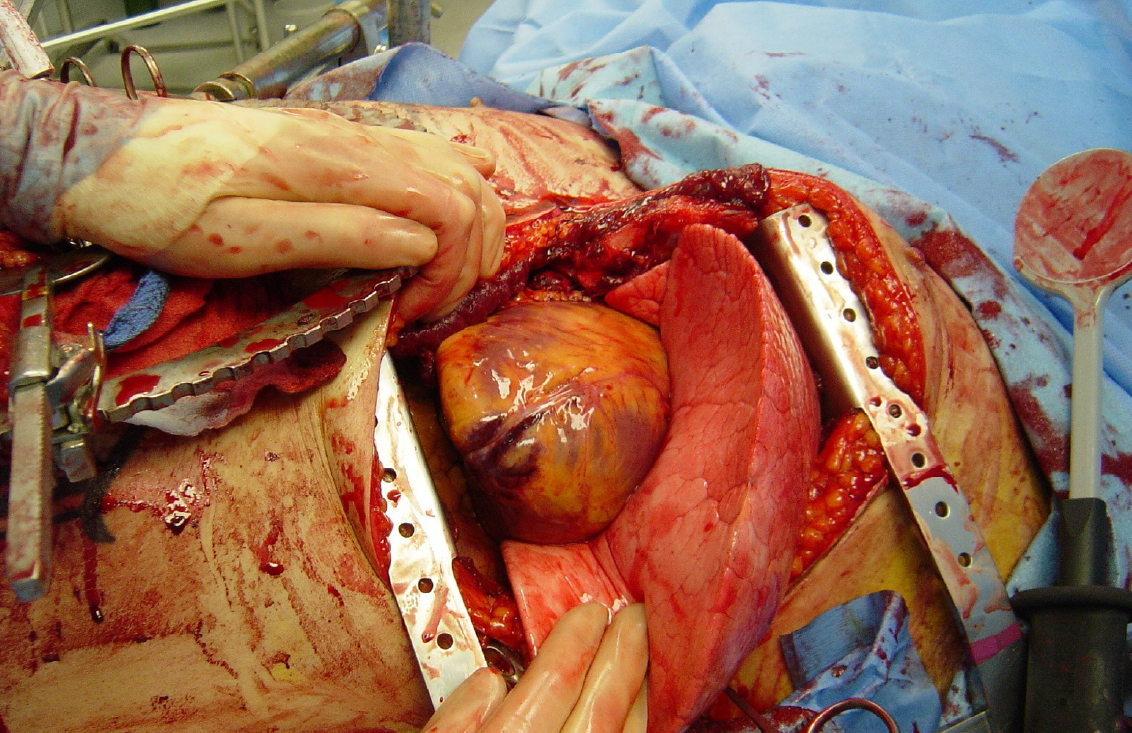
Operations on structures in the thorax generally involve thoracotomy. Severe pain frequently results from this surgical procedure. This acute post-thoracotomy pain appears to be the result of can result from trauma to the pleura, the associated musculature, costovertebral joint disruption, and injury to intercostal nerves during surgery. (Figure 3.)
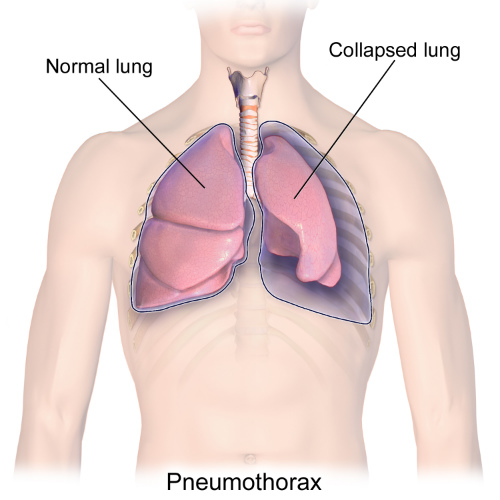
Many studies have established that poor intra-operative and postoperative analgesia can impede recovery and increase the risk complications such as pneumothorax (Figure 4) infection, and hematoma that result from ineffective respiration and clearing of secretions. Effective management of acute pain following thoracotomy may prevent these complications and reduce the likelihood of developing chronic pain.
A multi-modal approach to analgesia is widely employed by thoracic anesthetists using a combination of regional anesthetic blockade and systemic analgesia, with both non-opioid and opioid medications, and local nerve blocks. There is some evidence that blocking the nerves as they emerge from the spinal column (paravertebral block, PVB) may be associated with a lower risk of major complications in thoracic surgery. However, the majority of thoracic anesthetists continue to use a TEB analgesia for thoracotomy patients.
“In order to bring about a change in practice, anesthetists need a review that evaluates the risk of all major complications associated with thoracic epidural and paravertebral block in thoracotomy,” these reviewers advised.
The Analysis
The analysts conducted this systematic review in order to:
- Compare the techniques of TEB and PVB in adults undergoing elective thoracotomy;
- Evaluate the analgesic efficacy of the two techniques;
- Evaluate the incidence of major complications (including mortality);
- Examine the incidence of minor complications;
- Establish differences in length of hospital stay and cost effectiveness.
The reviewers were able to include all randomized controlled trials (RCTs) comparing PVB with TEB in thoracotomy, including upper gastrointestinal surgery. In all, 14 studies (n=698) were included.
There was low to very low-quality evidence that showed no significant difference in 30-day mortality (2 studies, 125 participants. risk ratio (RR) 1.28, 95% confidence interval (CI) 0.39 to 4.23, P=0.68) and major complications (cardiovascular: 2 studies, 114 participants. Hypotension RR 0.30, 95% CI 0.01 to 6.62, P=0.45; arrhythmias RR 0.36, 95% CI 0.04 to 3.29, P=0.36, myocardial infarction RR 3.19, 95% CI 0.13, 76.42, P=0.47); respiratory: 5 studies, 280 participants. RR 0.62, 95% CI 0.26 to 1.52, P=0.30).
The reviewers reported moderate-quality evidence that showing comparable analgesic efficacy across all time points both at rest and after coughing or physiotherapy (14 studies, 698 participants). There was moderate-quality evidence that showed PVB had a better minor complication profile than TEB including hypotension (8 studies, 445 participants. RR 0.16, 95% CI 0.07 to 0.38, P< 0.0001), nausea and vomiting (6 studies, 345 participants. RR 0.48, 95% CI 0.30 to 0.75, P=0.001), pruritus (5 studies, 249 participants. RR 0.29, 95% CI 0.14 to 0.59, P=0.0005) and urinary retention (5 studies, 258 participants. RR 0.22, 95% CI 0.11 to 0.46, P<0.0001).
They found insufficient data in chronic pain (6 or 12 months) and no difference in and length of hospital stay (3 studies, 124 participants). No studies reported differences in costs.
%20with%20PVB%20anesthesia%20can%20result%20in%20fewer%20postop%20complications%20pain%20cropped.jpg)
can result in fewer postop complications and lower pain scores.
Conclusions
“Paravertebral blockade reduced the risks of developing minor complications compared to thoracic epidural blockade. Paravertebral blockade was as effective as thoracic epidural blockade in controlling acute pain. There was a lack of evidence in other outcomes. There was no difference in 30-day mortality, major complications, or length of hospital stay,” the researchers concluded.
“There was insufficient data on chronic pain and costs. Results from this review should be interpreted with caution due to the heterogeneity of the included studies and the lack of reliable evidence. Future studies in this area need well-conducted, adequately-powered RCTs that focus not only on acute pain but also on major complications, chronic pain, length of stay and costs,” they added. (Figure 5.)
