The Myths of Dehydration and Heat Illnesses
- The primary cause of hyponatremia in athletes is drinking too much water.
- The incidence of hyponatremia appears to be between 13% and 15% among endurance athletes.
- Sodium supplementation has no effect on the occurrence of hyponatremia.
- There seems to not be a single case of death resulting from sports-related dehydration in the medical literature.
Every summer in the United States, athletes die and suffer neurologic complications from drinking too much. (See Figure.) The U.S. Army has seen the same result in a percentage of soldiers. The culprit is hyponatremia and the data suggest that the primary cause is simply drinking too much water.
Drinking Too Much
The rate of exercise-associated hyponatremia (EAH) has been reported at 15.1% among 887 finishers of a 100-mile (161-km) running race in Northern California. A study of runners in the 2002 Boston Marathon (27.2mi/43.8km) found 13% of 488 runners studied had hyponatremia (defined as a serum sodium concentration of ≤135mmol/L) and 0.6% had critical hyponatremia (serum sodium concentration of ≤120mmol/L) after finishing the race.
Currently, there is scientific agreement that overhydration resulting from drinking too much water is the primary cause of hyponatremia in athletes. Sodium supplementation appears to have no relationship with the occurrence of hyponatremia.
See a summary of the literature on this complex topic here.
Overweight and Obesity
The second most common causes of these deaths appear to be cardiac complications related to overweight and obesity. Heat deaths in the U.S. are more common in males and, according to Centers for Disease Control data from 2005-2009, the most recent data available, nearly 68% of those boys were overweight or obese.
The Myth of Dehydration
In the popular press, these heat-related deaths are often attributed to “heatstroke,” but no medical evidence is given. In other cases, if the death occurred under hot conditions, it is attributed to dehydration, but again, no medical evidence is given in these press reports. While dehydration can certainly be lethal, it is not clear how many of the deaths reported in the media are caused by dehydration. These cases were simply properly studied.
The rate of death due to dehydration in marathon and ultramarathon athletes appears to be unknown. This may be due to its exceedingly low rate. A PubMed search for “dehydration, athletes, death” returns 11 results. The strongest of these appears to be the Mortality and Morbidity Report referenced above. A search for “dehydration, runners, death,” returns 4 results. A review of these 15 studies reveals no case of death. There seems to not be a single case of death resulting from sports-related dehydration in the medical literature.
This report does not refer to death by dehydration at all. In each case it refers to heat-related injury. We have no way of knowing whether these injuries were due to dehydration, hyponatremia, heatstroke, elevated overall body temperature, cardiac, or other events.
Talk to Your Patients
While we still do not fully understand the effects of dehydration on athletes, it is much clearer that too much water kills and injures athletes. If hyponatremia is the most common cause of heat-related injury in athletes, suggestions to hydrate without limit can be injurious.
Caution endurance athletes to drink only when they are thirsty and to monitor their body weight before and after an event. Remind them that it is better to be thirsty than it is to be hyponatremic.
While the advice for patients is simple, the evidence is complicated, as you can see in our literature review on the topic.
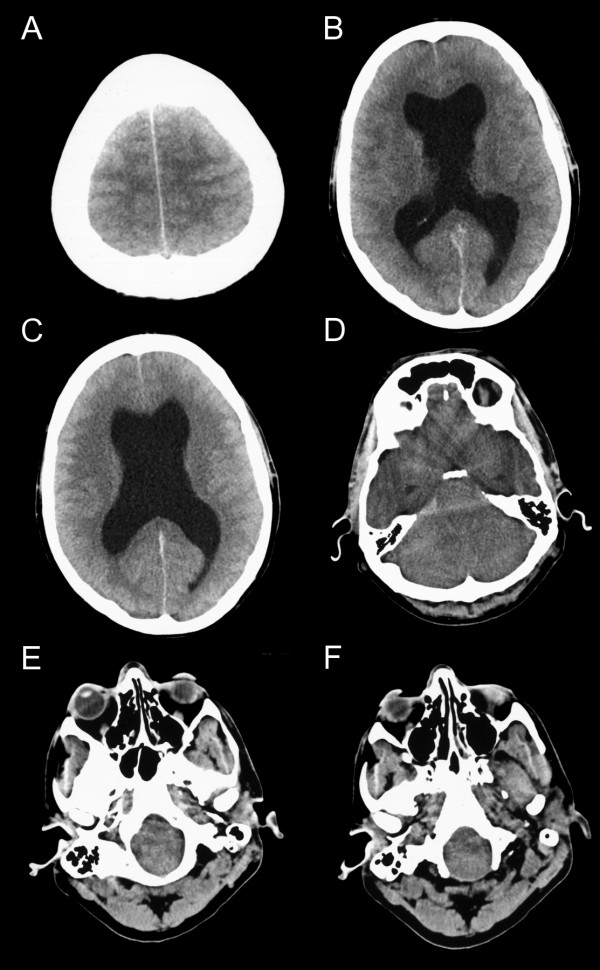
Figure: CT brain scan signs of hydrocephalus, high intracranial pressure and brain stem herniation. Brain CT (axial slices) in a male patient in his 30's who died of brain stem herniation after completing a marathon. The CT shows (A) loss of the rostral cerebral sulci suggesting increase in ICP, (B) and (C) a large hydrocephalus with widening of both temporal horns. The grey matter can still be differentiated from the white matter, but all sulci are lost. This suggests that the brain edema is of relative recent onset and massive tissue ischemia has not yet occurred. (D) Compression of the fourth ventricle with dilatation of the third ventricle and the caudal aspect of both temporal horns. This is observed with considerable brain edema and obstructive hydrocephalus. (E) Herniation of the medulla and pons into the foramen magnum. (F) The tonsils are located at the level of the dens which is a good indicator for foramen magnum herniation. (All images are from the case presented here.)
