—Annette Boyle, MDAlert.com contributing writer
- Obese patients who undergo bariatric surgery are 40% less likely to die at five and 10 years postop.
- Bariatric surgery significantly extends the lives of obese patients, even among older men with multiple comorbidities.
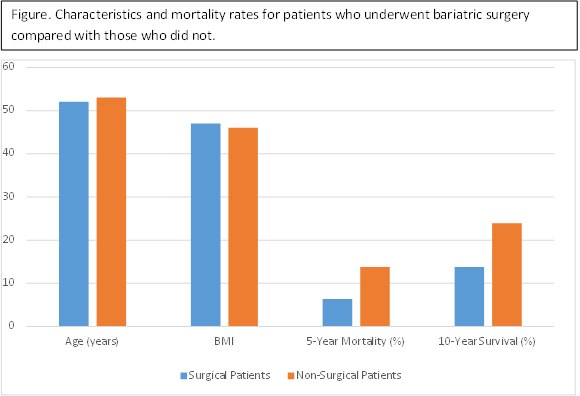
- Of the 10,000 patients studied, 74% were male and the average body mass index (BMI) among surgical patients was 47 compared to an average of 46 in nonsurgical patients.
A large study of Veterans Affairs patients published recently in JAMA has found that obese patients who undergo bariatric surgery are significantly less likely to die at five and 10 years following the procedure. This benefit was observed irrespective of age and a variety of comorbidities.
Adapted from: JAMA. 2015;313:62-70.
The new research shows that weight loss surgery—gastric bypass, gastrectomy, gastric banding or other—significantly extends the life of obese patients, even among older men with multiple comorbidities.
“Previous studies of long-term survival after bariatric surgery involved younger, mostly female populations who tended to have few obesity-related disease,” said David Arterburn, MD, MPH, a Group Health physician and University of Washington School of Medicine affiliate associate professor of medicine. “In contrast, our study’s population was older—with a mean age of 52—and 74% male. Also 55% of our population had diabetes, and many had other diseases such as high blood pressure, arthritis, heart disease, and depression.”
The average body mass index (BMI) among surgical patients was 47 compared to an average of 46 in nonsurgical patients.
In the study of nearly 10,000 patients published in the January issue of JAMA ( 2015;313:62-70), researchers found that those who underwent bariatric surgery at Veterans Affairs centers between 2000 and 2011 had mortality rates that were about 40% lower than matched controls at five and 10 years post-op (6.4% vs. 10.4% and 13.8% vs. 23.9%, respectively).
Adjusted analysis found no significant correlation between surgery and mortality rates in the first year. Those who underwent surgery had a 53% lower risk of all-cause mortality at five to 14 years following the procedure.
Given the growing number of severely obese Americans, the research provides good news for physicians eager to help patients avoid the myriad complications and comorbidities associated with a very high BMI.
“As time passes, the risk of dying among the patients who’ve had surgery appears to be diverging from those of the matched controls who haven’t had surgery,” Dr. Arterburn noted.
