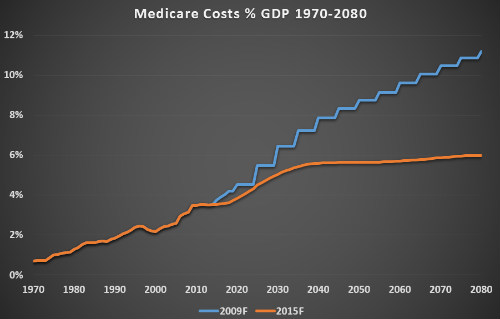
- In 2015, 80% of all Medicare spending will be on new, frequently curative treatments of hepatitis C (HCV) infection.
- Medicare spent about $7 million/y on older HCV drugs; will spend about $9 billion on new DAAs in 2015.
- Newer HCV drugs will be accompanied by high cost in the first few years of their use. A precipitous drop in spending is expected once the HCV epidemic is stemmed.
- HCV-related costs will drop sharply in the coming years, to below $2 billion by 2020, and to just $14 million by 2030.
- New DAAs are one of the greatest value propositions in the history of medicine; a fantastic value at a high up-front cost.
Sticker Shock
New direct acting antiviral (DAA) medications for treatment of hepatitis C (HCV) may present one of the greatest and most complex value propositions in the history of medicine. The number needed to treat is low with these drugs and some of the agents and combinations are curative in 99% to 100% of cases. However, the cost of the cure with any of the new medications has been reported to cost around $80,000.
The bigger cost picture today is this: Medicare’s cost of treating patients with HCV infections has skyrocketed from about $7 million before the introduction of DAAs (pre-2013, roughly) to approximately $9 billion in 2015.
Medicare spent about $4.5 billion last year on new DAAs. The fact that these drugs can cure hepatitis C was beginning to penetrate the medical consciousness. This was more than 15 times what Medicare spent the year before on older treatments for the disease, according to a widely reported release of previously undisclosed federal data. The release was reported upon by The Washington Post, PBS Newshour, the Associated Press, and U.S. News & World Report.
Are Direct-Active Antivirals a Good Value?
The essential question is whether these new drugs present a significant value at this price point. To answer this question, the clinician must consider the following, at least:
- Without DAAs, patients with HCV are chronically ill for life. There is no cap on how many healthcare resources they will consume.
- With DAA treatment, a chronically ill patient is often cured and ceases to cost the healthcare system anything at all. This could happen to the millions of people with HCV.
- Consider the improved quality of life for a patient who is cured vs. one who is chronically ill, in fear for his life, and in a state of constant decline.
- It stands to reason that cured patients would be more hopeful, less depressed, more engaged and responsible socially. One would expect that cured patients will, on average, be better parents, better spouses, friends, and brothers and sisters.
One of the Greatest Values in Medicine
The Post article acknowledges that “The new hepatitis C drugs have a higher cure rate—90% or higher—than previous treatments, as well as fewer harmful side effects. Some studies have shown that, despite their price tag, the drugs justify their cost based on the better quality of life they provide and the health expenses that patients avoid in the future.”
However the article makes no mention of the decreased cost of cured patients vs. patients who are chronically ill and, in many cases, getting sicker as the disease progresses. Many of these chronically ill HCV patients would come to need to undergo liver transplantation. Medicare would have to pay for this very costly procedure. Each transplantation procedure that is avoided by a cured case of HCV is a big saving for Medicare.
This value developed very quickly, explained Gyongyi Szabo, MD, PhD. “The cure of hepatitis C just 16 years after its identification is a credit to the field of hepatology,” she added. Dr. Szabo is President of the American Association for the Study of Liver Diseases (AASLD). She made these remarks in her President’s address to attendees of the 2015 annual meeting of the AASLD, held recently in San Francisco.
Progress Still to Make
Taking the promise of a cure to the point of making HCV a rare disease will require a significant investment, but one that would pay off quickly, according to a pair of studies by Jagpreet Chhatwal, PhD. Dr. Chhatwal presented the findings at the annual meeting of the AASLD.
Assuming that the number of noninstitutionalized individuals with HCV in the U.S. were to drop from 2 million today to 1 million by 2020 as a result of treatment with DAAs, the burden of HCV would remain high. “Under current management practices, 300,000 will die from HCV in the next 3 decades. This seems very high when we essentially have a cure for a disease,” Dr. Chhatwal said in an interview.
Before DAAs, the nation’s annual cost of HCV care approached $7 million per year. In 2015, it reached $21 billion and with HCV therapies driving almost 80% of that cost. According to Dr. Chhatwal, costs will drop sharply in the coming years, to below $2 billion by 2020 and to just $14 million by 2030. He estimated that it would cost $106 billion to make HCV a rare disease by 2040, an amount less than the U.S. spent on HIV/AIDS in the past 5 years alone.
