- Sepsis is common and it is one of the top killers in U.S. hospitals and worldwide.
- Since the definitions of sepsis and septic shock were last revised in 2001, considerable insights have been made into the pathobiology, management, and epidemiology of the syndromes.
- These important advances created sufficient need for reexamination of all related guidelines.
- The new paradigm excludes the of tachycardia, tachypnea, hyperthermia or hypothermia, and elevated white blood count sepsis diagnosis.
The Society of Critical Care Medicine (SCCM) has issued new guidelines for the definition, management, and treatment of sepsis and septic shock. These new guidelines include an in-depth review of the previous (2001) definitions and significant improvement both of definitions and guidance for management and treatment. The new guidelines were published at the 2016 annual meeting of the SCCM and in the Journal of the American Medical Association.
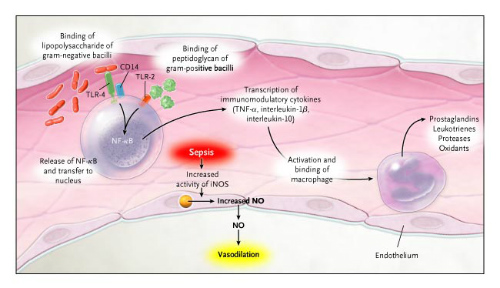
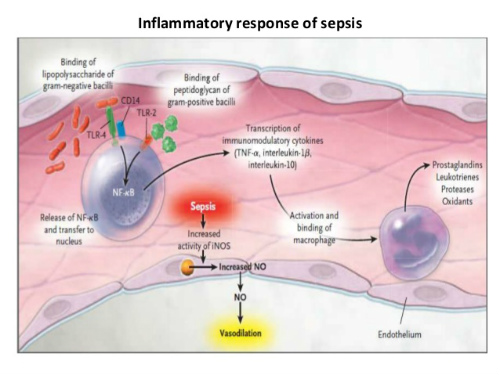
Since the definitions of sepsis and septic shock (Figures 1 and 2) were last revised in 2001, considerable insights have been made into the pathobiology, management, and epidemiology of the syndromes. These important advances created sufficient need for reexamination of all related guidelines.
The updated definitions of sepsis and septic shock eliminate criteria that have been shown to be nonspecific and have led to both misdiagnosis and overdiagnosis. The new definitions do away with the use of systemic inflammatory response syndrome (SIRS) criteria for the diagnosis of sepsis. The new paradigm excludes the of tachycardia, tachypnea, hyperthermia or hypothermia, and elevated white blood count sepsis diagnosis.
The Evaluation
Recent studies have shown that SIRS symptoms occur in a large majority of hospitalized patients and are often associated with conditions other than sepsis. “The SIRS criteria do not necessarily indicate a dysregulated, life-threatening response,” the task force wrote. “SIRS criteria are present in many hospitalized patients, including those who never develop infection and never incur adverse outcomes.”
“Sepsis is common and it is one of the top killers in U.S. hospitals and worldwide,” task force member Christopher W. Seymour, MD, of the University of Pittsburgh School of Medicine, said in an interview with MedPageToday.
“It has been almost two decades since a rigorous approach has been undertaken to better define sepsis and during that time a lot of new science has emerged examining the pathophysiology of sepsis, in particular how the body responds to it.”
These updated definitions and clinical criteria clarify long-used descriptors and facilitate earlier recognition and more timely management of patients with sepsis or at risk of developing sepsis developing it.
For instance, septic shock has been redefined to include sepsis with fluid-unresponsive hypotension, serum lactate level >2mmol/L, and the need for vasopressors to maintain mean arterial pressure ≥65mmHg.
In order to re-examine clinical definitions and responses to sepsis and septic shock, the researchers examined a cohort of 148,907 suspected sepsis infections. The analysis identified a rapid method—known as “quick SOFA” or qSOFA—for identifying suspected sepsis.
The Quick SOFA Method
When the qSOFA method was put to use, 25% patients who had 2 or more positive of the three symptoms accounted for 70% of all sepsis cases. The qSOFA model quickly identified the sickest patients who would then go on to undergo the full battery of laboratory tests to confirm sepsis.
The SCCM task force recommended that the qSOFA criteria be used to prompt clinicians “to further investigate for organ dysfunction, to initiate or escalate therapy as appropriate, and to consider referral to critical care or increase the frequency of monitoring.”
“The task force considered that positive qSOFA criteria should also prompt consideration of possible infection in patients not previously recognized as infected,” they wrote. (Figure 3.)

New Definitions: Sepsis and Septic Shock
Sepsis
Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection. “This new definition emphasizes the primacy of the nonhomeostatic host response to infection, the potential lethality that is considerably in excess of a straightforward infection, and the need for urgent recognition,” the task force wrote. Even a modest degree of organ dysfunction when infection is first suspected is associated with an in-hospital mortality rate in excess of 10%, they noted.
The Task force recommended that “sepsis should be defined as life-threatening organ dysfunction caused by a dysregulated host response to infection. For clinical operationalization, organ dysfunction can be represented by an increase in the Sequential [Sepsis-related] Organ Failure Assessment (SOFA) score of 2 points or more, which is associated with an in-hospital mortality greater than 10%.”
Septic Shock
“Septic shock should be defined as a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone,” the advisors wrote.
The 2016 task force proffered a broader view to differentiate septic shock from cardiovascular dysfunction alone and to recognize the clinical importance of cellular dysfunction. The task force was unanimous in its agreement that “septic shock should reflect a more severe illness with a much higher likelihood of death than sepsis alone.”
The revised definition categorizes patients with septic shock as those who are not hypovolemic but require vasopressors in order to maintain a mean arterial pressure (MAP) of ≥65mmHg and serum lactate level >2 mmol/L (>18 mg/dL). Importantly, the combination of MAP of ≥65mmHg and serum lactate level >2 mmol/L has been associated with in-hospital mortality rates >40%.
Outside of a hospital, emergency department, or general hospital ward setting, adult patients with suspected infection can be rapidly identified as being at high risk if they have >2 of the following clinical criteria:
- Respiratory rate of 22/min or greater,
- Altered mentation
- Systolic blood pressure of ≤100mmHg
The new recommendations define septic shock as a “subset of sepsis in which underlying circulatory, cellular and metabolic abnormalities are associated with a greater risk of mortality than sepsis alone.” Within this paradigm, adult patients can be identified as suffering from septic shock if they have a degree of hypotension that requires vasopressor therapy to maintain mean blood pressure of 65mmHg or greater and having a serum lactate level greater than 2mmol/L after adequate fluid resuscitation.
Conclusions
These updated definitions and clinical criteria should replace previous definitions, offer greater consistency for epidemiologic studies and clinical trials, and facilitate earlier recognition and more timely management of patients with sepsis or at risk of developing sepsis.
These updated definitions and clinical criteria should clarify long-used descriptors and facilitate earlier recognition and more timely management of patients with sepsis or at risk of developing it. This process, however, remains a work in progress. As is done with software and other coding updates, the task force recommends that the new definition be designated Sepsis-3, with the 1991 and 2001 iterations being recognized as Sepsis-1 and Sepsis-2, respectively, to emphasize the need for future iterations.
