- Surgical meniscus repair was not superior to sham surgery in a randomized, controlled trial.
- Non-surgical care of meniscus-injury related pain, such as exercise, was equally or more effective than surgical interventions.
- Approximately 700,000 arthroscopic partial meniscectomies are performed annually in the U.S.
- Annual direct medical costs are estimated at $4 billion.
- Physicians and patients should consider all non-surgical options before undertaking surgical intervention for knee pain related to meniscus injury.
Approximately 700,000 arthroscopic partial meniscectomies are performed annually in the U.S. Annual direct medical costs are estimated at $4 billion. However, the surgery has been found to be no more effective than sham surgery, simply ineffective, unnecessary, and dangerous in a number of studies.
Arthroscopic repair of meniscal tear (Figure 1) was found to be no more effective than non-operative management as a first-line therapy for patients with knee pain and a degenerative meniscal tear, according to the results of a systematic review published recently in the American Journal of Sports Medicine.
The authors of a meta-analysis published in the Archives of Orthopaedic and Trauma Surgery came to a similar conclusion based on Level 1 data: “This meta-analysis illustrates the lack of level I evidence to guide the surgical management of meniscal tears,” the authors concluded.
Results of a randomized, controlled trial published in the British Journal of Medicine also found no significant differences between surgical and nonsurgical approaches to the treatment of meniscal injuries patients who had no evidence of osteoarthritis.
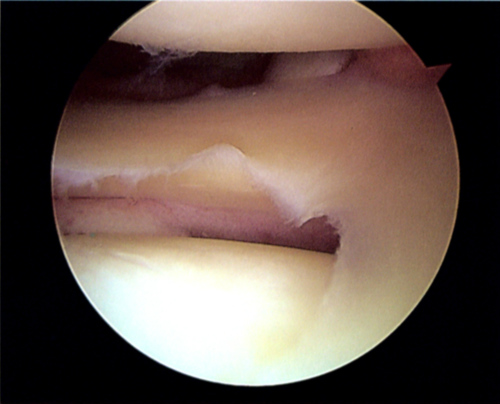
of the image, extends to the center of the image, and continues to the lower middle
of the image. The feather-like structures are fragments of cartilage.
(Source: Wikipedia/By Tim1965/Creative Commons.)
Surgical Repair vs. Sham Surgery
In fact, a study published in The New England Journal of Medicine compared outcomes of arthroscopic partial meniscus repair (Figure 2) with sham surgery in a randomized, controlled trial. A total of 146 patients were randomly assigned to undergo either arthroscopic partial meniscectomy (n=70) or sham surgery (n=76).
“The results of this randomized, sham-controlled trial show that arthroscopic partial medial meniscectomy provides no significant benefit over sham surgery in patients with a degenerative meniscal tear and no knee osteoarthritis. These results argue against the current practice of performing arthroscopic partial meniscectomy in patients with a degenerative meniscal tear,” the authors concluded.
Strong data suggest that surgical meniscal repair
is ineffective, dangerous, and expensive.

following surgery for a tear in the meniscus.
(Sources: Wikipedia/By Tim1965/Creative Commons.)
British Journal of Medicine
A study published recently in the British Journal of Medicine was designed to determine whether exercise therapy is superior to arthroscopic partial meniscectomy for knee function in middle aged patients with degenerative meniscal tears.
The authors concluded that “The observed difference in treatment effect was minute after two years of follow-up, and the trial’s inferential uncertainty was sufficiently small to exclude clinically relevant differences. Exercise therapy showed positive effects over surgery in improving thigh muscle strength, at least in the short term. Our results should encourage clinicians and middle aged patients with degenerative meniscal tear and no definitive radiographic evidence of osteoarthritis to consider supervised exercise therapy as a treatment option.”
This randomized, controlled superiority trial included 140 adults with a mean age 49.5 years (range 35.7-59.9). Patients had degenerative medial meniscal tear verified by magnetic resonance imaging; 96% had no definitive radiographic evidence of osteoarthritis.
Patients were randomly assigned to one of 2 interventions: 12 week supervised exercise therapy (Figure 3) alone or arthroscopic partial meniscectomy alone.
The main outcomes were intention to treat analysis of between-group difference in change in knee injury and osteoarthritis outcome score (KOOS4), defined a priori as the mean score for 4 of 5 KOOS subscale scores (pain, other symptoms, function in sport and recreation, and knee related quality of life). Outcomes were measured from baseline to 2-year follow-up and change in thigh muscle strength from baseline to 3 months.
The authors found no clinically relevant differences between the 2 groups in change in KOOS4 at 2 years (0.9 points, 95% confidence interval −4.3 to 6.1; P=0.72). At 3 months, muscle strength had improved in the exercise group (P≤0.004). No serious adverse events occurred in either group during the 2-year follow-up; 19% of the participants allocated to exercise therapy crossed over to surgery during the 2-year follow-up but received no additional benefit.

(Sources: Wikipedia/By Vinceypo0 (Own work)/Wikimedia Commons/Creative Commons.)
American Journal of Sports Medicine
Because arthroscopic surgery of the knee is one of the most frequently performed orthopedic procedures, and approximately 30% of these procedures are performed to repair meniscal injuries (Figure 4), the author of this meta-analysis published in the American Journal of Sports Medicine sought to identify which surgical interventions actually improved patient’s conditions.
The authors performed an online search of randomized, controlled trials (RCTs) and systematic reviews (SRs) that compared treatment options for meniscal injury. The reviewers included articles published in the CENTRAL; MEDLINE; EMBASE; NHS Evidence; National Guideline Clearing House, Database of Abstracts of Reviews of Effects, Health Technology Assessment; ISRCTN; Clinicaltrials.gov; and WHO trials databases.
The reviewers analyzed 9 RCTs and 8 SRs. The studies revealed no differences in outcomes between arthroscopic meniscal debridement and nonoperative management as a first-line treatment strategy for patients with knee pain and a degenerative meniscal tear (mean difference: Knee injury and Osteoarthritis Outcome Score, 1.6 [95% CI, -2.2 to 5.2], pain Visual Analogue Scale score, -0.06 [95% CI, -0.28 to 0.15]).
“Some evidence was found to indicate that patients with resistant mechanical symptoms who initially fail nonoperative management may benefit from meniscal debridement No studies compared meniscal repair with meniscectomy or nonoperative management. Initial evidence suggested that meniscal transplant might be favorable in certain patient groups,” they noted.
“Further evidence is required to determine which patient groups have good outcomes from each intervention. Given the current widespread use of arthroscopic meniscal surgeries, more research is urgently needed to support evidence-based practice in meniscal surgery in order to reduce the numbers of ineffective interventions and support potentially beneficial surgery,” the reviewers concluded.
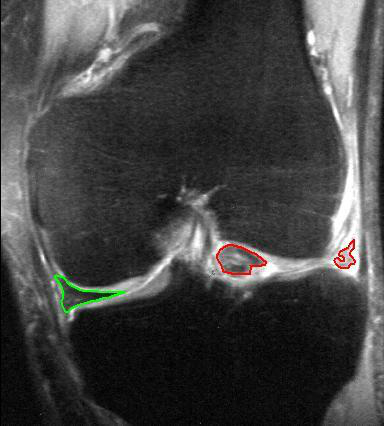
MRI, coronal T2 *-weighted GRE sequence.
(Source: Wikipedia/By MBq/Public Domain via Wikipedia Commons.)
Archives of Orthopaedic and Trauma Surgery
The reviewers who authored the study published in the Archives of Orthopaedic and Trauma Surgery also endeavored to compare the outcomes of various surgical treatments for meniscal injuries including:
- Total and partial meniscectomy;
- Meniscectomy and meniscal repair;
- Meniscectomy and meniscal transplantation;
- Open and arthroscopic meniscectomy and
- Various different repair techniques.
The reviewers examined The Bone, Joint and Muscle Trauma Group Register, Cochrane Database, MEDLINE, EMBASE and CINAHL for “all (quasi) randomized controlled clinical trials comparing various surgical techniques for meniscal injuries. Primary outcomes of interest included patient-reported outcomes scores, return to pre-injury activity level, level of sports participation and persistence of pain using the visual analogue score. Where possible, data were pooled and a meta-analysis was performed.”
The review included a total of 9 studies involving a 904 patients. Of these, 330 underwent a meniscal repair, 402 had a meniscectomy, and 160 received a collagen meniscal implant. “The only surgical treatments that were compared in homogeneous fashion across more than one study were the arrow and inside-out technique, which showed no difference for re-tear or complication rate. Strong evidence-based recommendations regarding the other surgical treatments that were compared could not be made,” the authors noted.
The New York Times
The New York Times recently weighed in on this issue in two separate articles. The Times quoted an editorial that accompanied the publication of the RCT in The British Medical Journal. “An accompanying editorial came to a scathing conclusion: The surgery is ‘a highly questionable practice without supporting evidence of even moderate quality,’ adding, ‘Good evidence has been widely ignored.’”
Gordon H. Guyatt, MD, Professor of Medicine and Epidemiology at McMaster University in Hamilton, Ontario, wrote the editorial in The British Medical Journal.
“I personally think the operation should not be mentioned,” he told The Times. “We have randomized clinical trials that produce the highest quality of evidence. They strongly suggest that the procedure is next to useless. If there is any benefit, it is very small and there are downsides, expense, and potential complications.’”
Additionally: Jeffrey N. Katz, MD, a Professor of Medicine and Orthopedic Surgery at Harvard Medical School, explained in The Times article that not everyone improves after the surgery. “’It is not regarded as a slam-dunk,” he said. As a result, he said, many doctors have been genuinely uncertain about which is better—exercise and physical therapy or surgery. That, in fact, was what led Dr. Katz and his colleagues to conduct a clinical trial comparing surgery with physical therapy in middle-aged people with a torn meniscus and knee pain.
Physicians should consider each case deeply before they recommend surgical meniscus repair to a patient. The opportunities for improved patient care, improved patient outcomes, and non-surgical billing are much greater when physicians offer non-operative care for knee pain.
