Triplet Therapy Shrinks HER2-Positive Gastric Cancer Tumors
By Michael Vlessides, /alert Contributor
February 5, 2021
Updated results from an international, multi-center investigation have revealed that first-line triplet therapy with pembrolizumab, trastuzumab, and chemotherapy has promising efficacy in patients with HER2-positive advanced gastric cancer.
The study found that patients receiving the drug combination experienced clinically meaningful improvements in tumor shrinkage regardless of PD-L1 status, with no new safety signals.
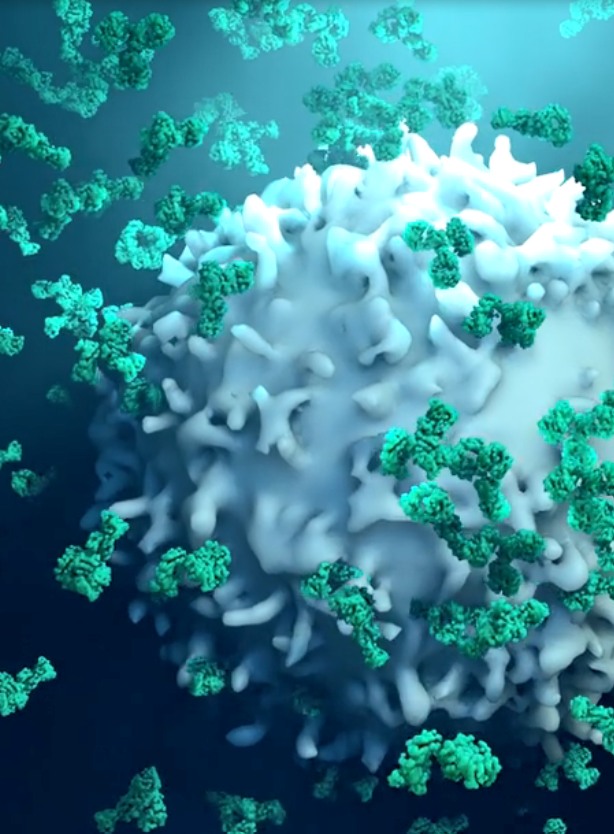
Presenting at the 2021 Gastrointestinal Cancers Symposium of the American Society of Clinical Oncology (abstract 218), the authors explained that previous research has demonstrated the immune system’s substantial contributions to trastuzumab’s therapeutic effects in solid tumors. For its part, pembrolizumab is a potent, highly selective humanized monoclonal antibody that blocks the interaction between PD-1 and its ligands, PD-L1 and PD-L2.
As such, the researchers embarked on the so-called PANTHERA trial (NCT02901301), a phase 1B/2 study to determine the safety and anti-tumor activity of pembrolizumab in combination with a standard therapeutic regimen of trastuzumab, capecitabine, and cisplatin among individuals with HER2 positive gastric cancer.
The trial comprised 43 such patients, all of whom were treated with 200 mg intravenous pembrolizumab (day 1), 6 mg/kg trastuzumab (day 1; after an 8mg/kg load), 1000 mg/m2 twice-daily capecitabine (days 1-14), and 80 mg/m2 cisplatin (day 1) every three weeks. The primary endpoint was objective response rate per RECIST v1.1. Secondary endpoints included progression-free survival, overall survival, duration of response, safety, and predictive biomarker analysis by targeted next generation sequencing.
Median follow-up among the study’s 43 participants was 18.2 months; six patients completed two years of treatment without disease progression. Objective response rate was found to be 76.7%; 26 patients (56.6%) demonstrated a reduction in tumor burden of at least 50%.
Median progression-free survival was found to be 8.6 months (95% CI: 7.2-16.4 months), while median overall survival was 19.3 months (95% CI: 16.5 months-not reached). Patients who received the combination therapy also had an overall response rate of 76.7% (95% CI: 61.4-88.2%) and a disease control rate of 97.7% (95% CI: 87.7-99.9%).
According to lead author Sun Young Rha, MD, PhD, a medical oncologist in the Division of Medical Oncology at Yonsei Cancer Center in Seoul, South Korea, clinical parameters -- including PD-L1 status -- were not related to survival.
Biomarker analyses were performed on 98 tumor tissue samples from 39 patients, which were analyzed with targeted next genome sequencing. Interestingly, these analyses found that baseline HER2 amplification was related to survival. Indeed, median progression-free survival was 22 months among individuals with HER2 amplification, compared with 7.7 months among their counterparts without HER2 amplification (p=0.0275). Similar results were found in patients with altered RTK/RAS pathways, who had significantly longer median progression-free survival (13.8 months) than did those with wild-type RTK/RAS (4.9 months; p=0.001).
No patients discontinued pembrolizumab because of immune-related adverse events.
“In summary,” Rha concluded, “first-line triplet regimen pembrolizumab, trastuzumab, and chemotherapy showed promising efficacy based on HER2 amplification by NGS regardless of PD-L1 status in advanced gastric cancer. Correlative biomarkers found from our study need to be validated through ongoing trials.”
Such validation, she added, will likely occur in the ongoing phase 3 KEYNOTE-811 study (NCT03615326).


.jpg)