- The Affordable Care Act (ACA) levies fines for readmission rates that are above a benchmark, according to a study published in the New England Journal of Medicine.
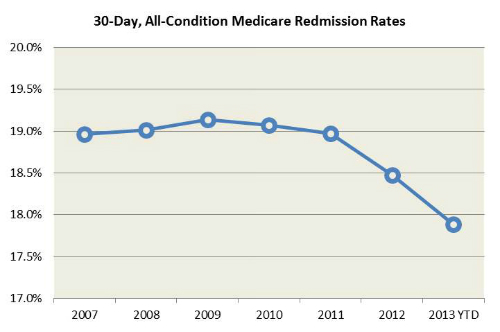
- Rates of readmission have declined for both targeted and nontargeted conditions since implementation of the ACA.
- From 2007 to 2015, readmission rates for targeted conditions declined from 21.5% to 17.8%, and rates for nontargeted conditions declined from 15.3% to 13.1%.
Readmission rates have fallen since the implantation of the Affordable Care Act (ACA) was implemented (Figures 1 and 2), according to a study published recently in the New England Journal of Medicine. The readmissions trends are consistent with hospitals’ responding to incentives to reduce readmissions, including the financial penalties for readmissions levied as part of the ACA. “We did not find evidence that changes in observation-unit stays accounted for the decrease in readmissions,” the authors concluded
since implementation of the Affordable Care Act.
have fallen since implementation of the Affordable Care Act.
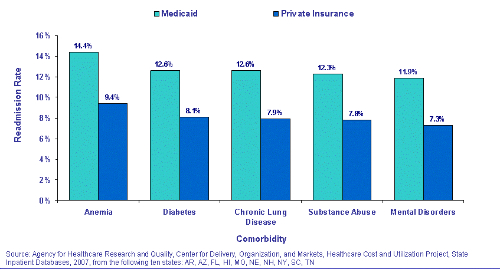
The Hospital Readmissions Reduction Program is part of the ACA. It institutes financial penalties for hospitals that have readmission rates that are above a benchmark set point for targeted conditions. “Some policy analysts worry that reductions in readmissions are being achieved by keeping returning patients in observation units instead of formally readmitting them to the hospital. We examined the changes in readmission rates and stays in observation units over time for targeted and nontargeted conditions and assessed whether hospitals that had greater increases in observation-service use had greater reductions in readmissions,” the authors explained.
The Analysis
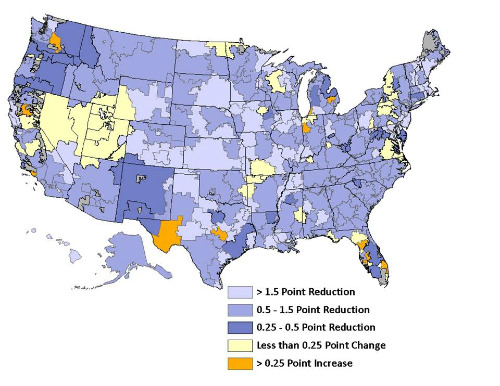
The authors compared monthly, hospital-level rates of readmission and observation-service use within 30 days after hospital discharge among Medicare elderly beneficiaries from October 2007 through May 2015. Using an interrupted time-series model they determined when trends changed and whether changes differed between targeted and nontargeted conditions. Targeted conditions include heart attacks, heart failure, and pneumonia. Readmission rates still vary geographically in the U.S. (Figure 3.)
The included data from 3387 hospitals. Readmission rates for targeted conditions declined from 21.5% to 17.8%, and rates for nontargeted conditions declined from 15.3% to 13.1% between 2007 and 2015. Shortly after passage of the ACA, the readmission rate declined quickly, especially for targeted conditions, and then continued to fall at a slower rate after October 2012 for both targeted and nontargeted conditions, the authors noted.
Stays in observation units for targeted conditions increased from 2.6% in 2007 to 4.7% in 2015, and rates for nontargeted conditions increased from 2.5% to 4.2%. Within hospitals, there was no significant association between changes in observation-unit stays and readmissions after implementation of the ACA. Readmission rates fell more sharply for conditions that were targeted by the Hospital Readmissions Reduction Program than for other conditions requiring hospitalizations, such as surgeries and diabetes. The number of observation stays was found to be very small compared to actual hospital readmissions. These have increased steadily since 2008 but with no acceleration after the ACA was enacted.
