Study Findings Show Imbalance Between Clinical and Real-World CLL Treatment With Idelalisib
By Adam Hochron
April 14, 2020
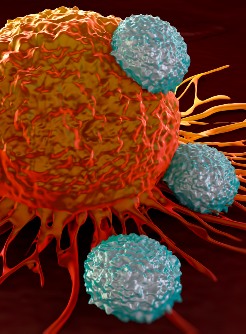
Successful clinical trials may not always guarantee success outside of the lab. A recent study looked at this issue involving the use of idelalisib for patients with relapsed follicular lymphoma and chronic lymphocytic leukemia.
The study compared the results of patients in two clinical trials with Medicare patients with the same condition as those in the studies. The success of treatment was based on three factors: treatment duration, on-treatment and overall mortality, and serious and fatal infections. Results of the study were published in JAMA Oncology..jpg)
Idelalisib, an oral phosphatidylinositol 3-kinase inhibitor, is approved by the FDA for relapsed chronic lymphocytic leukemia in combination with rituximab. It also received accelerated approval for relapsed follicular B-cell non-Hodgkin lymphoma and relapsed small lymphocytic lymphoma after two or more prior therapies.
“Although trials supporting [idelalisib] approval had an acceptable risk-benefit profile, 7 subsequent trials were halted in March 2016, for a higher incidence of serious and fatal adverse events in patients treated with [idelalisib],” the authors said.
In looking at the data, comparing 115 clinical trial patients with 599 Medicare patients, the authors noted that those treated in the real world were “older, sicker, and had unfavorable imbalances in treatment duration, mortality, and fatal infections compared with clinical trial participants."
For infection rates, the fatal infection rate per 100 person-years was “significantly higher” for the Medicare patients in the study than those in clinical trials who were treated with [idelalisib] and rituximab for CLL (18.4 vs 9.8, P = .04), and “numerically higher” for patients treated with [idelalisib] for FL (27.6 vs 18.6, P = .54). The authors also noted that infection rates were higher in the first six months than the rest of the study time, with pneumonia and sepsis regularly observed.
"Immunosuppression-related toxic effects, including infection, may have been somewhat reduced in trials by more frequent dose reductions and exclusion of patients with ongoing infections,” the authors said in their conclusion. “Selective eligibility criteria and closer monitoring of trial patients may be responsible for limited generalizability of trial data to clinical practice.”












.jpg)





.jpg)





.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)