Pembrolizumab Improves PFS for Patients With Relapsed, Refractory Classical Hodgkin Lymphoma
By Cameron Kelsall, /alert Contributor
April 5, 2021
Pembrolizumab provided a statistically significant improvement in progression-free survival (PFS) when compared with brentuximab vedotin for the treatment of patients with relapsed or refractory classical Hodgkin lymphoma, according to an interim analysis of the phase 3 KEYNOTE-204 study published in The Lancet Oncology.
Patients with relapsed or refractory classical Hodgkin lymphoma often face poor outcomes if their disease progresses following autologous hematopoietic stem cell transplant (HSCT), or if they are transplant ineligible. Brentuximab vedotin is an approved standard of care for these patients, but its ability to extend PFS remains limited, and more than 40% of patients experience peripheral neuropathy.
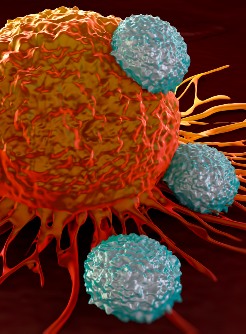
“PD-L1 and PD-L2 are overexpressed on tumor cell surfaces in classical Hodgkin lymphoma and are therefore attractive therapeutic targets for this disease,” wrote John Kuruvilla, MD, FRCPC, clinician investigator at Princess Margaret Cancer Centre (Toronto, ON), and colleagues. “Two anti–PD-1 antibodies are currently approved in classical Hodgkin lymphoma, pembrolizumab and nivolumab, and both have been found to provide long-term efficacy in patients with relapsed or refractory classical Hodgkin lymphoma.”

Kuruvilla and colleagues conducted an international, open-label, randomized study comparing pembrolizumab and brentuximab in adult patients with relapsed or refractory classical Hodgkin lymphoma. The study included patients who relapsed following an autologous HSCT and transplant-ineligible patients.
The researchers randomly assigned patients to intravenous pembrolizumab (200 mg every 3 weeks) or intravenous brentuximab vedotin (1.8 mg/kg every 3 weeks). They stratified randomization based on previous transplant status (yes vs. no) and status after frontline therapy (primary refractory vs. relapsed <12 months after frontline therapy vs. relapsed ≥12 months after frontline therapy).
Treatment continued until disease progression, unacceptable toxicity, investigator decision or the completion of 35 cycles. Pembrolizumab dose reductions were not permitted.
PFS by blinded independent central review and overall survival served as the study’s dual primary endpoints. The interim analysis did not report overall survival data, as the number of required events had not been reached.
The study included data from 304 patients (pembrolizumab, n = 151; brentuximab vedotin, n = 153), of whom 37% (n = 112) underwent previous autologous HSCT and 63% (n = 192) were transplant ineligible. The median time from randomization to data cutoff for this analysis was 25.7 months (interquartile range [IQR], 23.4-33).
Patients assigned pembrolizumab had a median duration of treatment of 305 days (IQR, 131.5-635), compared with 146.5 days (IQR, 65-232.5) for patients assigned brentuximab vedotin. The median number of treatment cycles were 15 (IQR, 7-30.5) for pembrolizumab and 7 (IQR, 4-12) for brentuximab vedotin.
Median PFS significantly favored treatment with pembrolizumab over brentuximab vedotin (13.2 months vs. 8.3 months; hazard ratio [HR], 0.65; 95% CI, 0.48-0.88; P = .0027).
The median duration of response among responding patients was 20.7 months (95% CI, 12.4 months to not reached) in the pembrolizumab arm and 13.8 months (95% CI, 5.8 months to not reached) in the brentuximab vedotin arm. In total, 48 patients assigned pembrolizumab and 23 patients assigned brentuximab vedotin had a response lasting at least 12 months.
The safety analysis included all patients who received at least one dose of their assigned study drug. Treatment-related adverse events occurred in 74% (n = 110) of the pembrolizumab arm and 77% (n = 117) of the brentuximab vedotin arm.
The most common grade 3-5 treatment-related adverse events were pneumonitis (pembrolizumab vs. brentuximab vedotin, 4% vs. 1%), neutropenia (2% vs. 7%), decreased neutrophil count (1% vs. 5%) and peripheral neuropathy (1% vs. 3%). Serious adverse events occurred in 16% (n = 24) of the pembrolizumab arm and 11% (n = 16) of the brentuximab vedotin arm.
Three patients in the pembrolizumab arm and two patients in the brentuximab vedotin arm died due to adverse events. The researchers deemed one death due to pneumonia in the pembrolizumab arm as related to treatment.
In addition, 19 patients assigned pembrolizumab and 25 patients assigned brentuximab vedotin discontinued treatment due to adverse events.
“[R]esults from the KEYNOTE-204 study suggest that pembrolizumab should be considered the preferred treatment option for patients with relapsed or refractory classical Hodgkin lymphoma who have relapsed after autologous HSCT or are ineligible for autologous HSCT,” the researchers concluded.












.jpg)





.jpg)





.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)