Immunotherapy Combination Offers No Benefit in R/R Lymphoid Cancers
By Andrew John, /alert Contributor
May 4, 2021
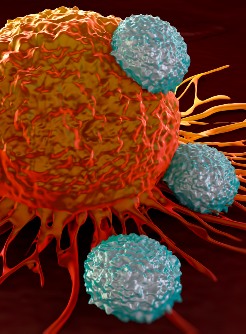
Combining nivolumab with a CTLA-4 or KIR blockade in the form of ipilimumab or lirilumab did not confer any significant improvement compared with nivolumab alone in patients with relapsed or refractory lymphoid cancers, according to study data.
The phase 1b study was an extension of the phase 1 CheckMate 039 study, which examined nivolumab in patients with relapsed or refractory multiple myeloma, classical Hodgkin lymphoma, or non-Hodgkin lymphoma.
“Simultaneously targeting other pathways could increase the activity of PD-1 blockade in lymphoid malignancies not sensitive to single-agent blockade,” Philippe Armand, MD, PhD, chief of the Division of Lymphoma in the Department of Medical Oncology at the Dana-Farber Cancer Institute, and colleagues wrote. “We explored the safety and efficacy of combined PD-1 and CTLA-4 or KIR blockade in patients with relapsed/refractory lymphoid malignancies.”
The researchers performed a multicohort study of patients aged 18 years and older with relapsed or refractory multiple myeloma, classical Hodgkin lymphoma, or non-Hodgkin lymphoma. Armand and colleagues excluded patients with lymphoblastic or Burkitt lymphoma. The main outcomes were tolerability and safety. Secondary outcomes included progression-free and overall survival rates, as well as overall and complete responses rates.
In the cohort assigned to nivolumab and ipilimumab, patients (n = 65) received 3 mg/kg intravenous nivolumab and 1 mg/kg ipilimumab on the first day of each three-week cycle. Then, after four cycles of this regimen, they received nivolumab alone at 3 mg/kg on the first and fifteenth days of each four-week cycle. Patients assigned to nivolumab and lirilumab (n = 72) received nivolumab at 3 mg/kg on the first and fifteenth day of each four-week cycle, and intravenous lirilumab at 3 mg/kg on the first day of each cycle. Researchers continued treatment for both cohorts until progressive disease, unacceptable toxicity, complete remission, or for up to two years.
Among patients who had classical Hodgkin lymphoma, those assigned to nivolumab and ipilimumab had an overall response rate of 74%, compared with 76% in those assigned to nivolumab and lirilumab, the researchers reported. The complete response rate for patients with classical Hodgkin lymphoma was 23% for ipilimumab and 24% for lirilumab.
The complete response rate in those with B- or T- non-Hodgkin lymphoma ranged from zero to 6%, while the overall response rate ranged from 9% to 22%.
Armand and colleagues wrote that there was no objective response in any of the patients with multiple myeloma.
In the ipilimumab group, 29% of patients experienced grade 3 or 4 adverse events, compared with 15% in the lirilumab group. Researchers reported greater toxicity in the ipilimumab group than would be expected from monotherapy with nivolumab.
“...The present data do not suggest that those combinations meaningfully improve the already strong therapeutic activity of nivolumab in cHL, nor do they suggest that the combinations provide a significant therapeutic benefit in unselected B-non-Hodgkin lymphoma, T-non-Hodgkin lymphoma, or multiple myeloma populations … emphasizing that this conclusion relies on a small number of patients,” the researchers wrote.
Disclosures: Armand reports consulting roles with Adaptive, ADC Therapeutics, Affimed, Bristol Myers Squibb, Celgene, Daiichi Sankyo, Infinity, Merck, Miltenyi, Morphosys and Pfizer; institutional research funding from Adaptive, Affimed, Bristol Myers Squibb, Genentech, IGM, Merck, Otsuka, Roche, Sigma Tau and Tensha; and honoraria from Bristol Myers Squibb and Merck. Please see the full study for a complete list of all other authors’ relevant financial disclosures.











.jpg)





.jpg)





.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)