Click here for the next report.
San Francisco—For patients with HCV, the presence of decompensated liver disease significantly complicates treatment and increases morbidity and mortality. In phase 2 trials, the combination of velpatasvir and sofosbuvir achieved sustained virologic response 12 weeks post treatment for 99% patients with all 5 HCV genotypes.
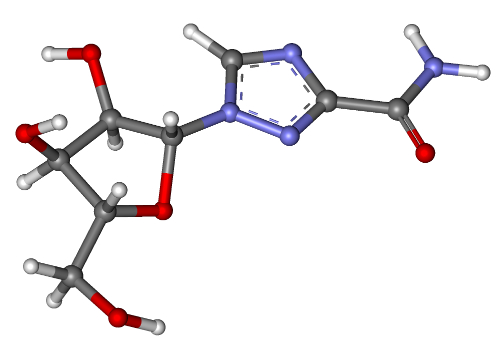
The phase 3 study found that a fixed dose of 100 mg velpatasvir and 400 mg sofosbuvir plus ribavirin produced an overall sustained virologic response rate 12 weeks post treatment of 94.3% in patients with decompensated liver disease. This is a greater than 10% improvement over the results seen when using only the combination of velpatasvir and sofosbuvir alone for 12 or 24 weeks. MR Charlton, et al, reported the findings as Late Breaking abstract 13 (LB-13) at the 2015 annual meeting of the AASLD. You can find the entire abstract here.
At the start of the study, the median Child-Pugh-Turcotte (CPT) score was 8 and the median Model for End-stage Liver Disease (MELD) score ranged from 6 to 24. About half of patients who achieved sustained virologic response also saw improvements in CPT (47%) and MELD scores (56%) by week 12 post treatment.
The study included 267 patients with genotypes 1, 2, 3, 4 or 6 HCV infections who were randomized to 12 weeks of velpatasvir/sofosbuvir, 12 weeks of velpatasvir/sofosbuvir plus ribavirin or 24 weeks of velpatasvir/sofosbuvir. Participants were predominantly male (70%), white (90%) and treatment experienced (55%) and 78% had genotype 1 infections.
Relapses occurred in one genotype 1 patient and one genotype 3 patient on the velpatasvir/sofosbuvir plus ribavirin therapy. An additional genotype 3 patient experienced on-treatment breakthrough with lab value that indicated non-adherence. No treatment failures occurred in genotype 2, 4 or 6 patients in any of the study arms. Nine patients discontinued treatment due to adverse events, including sepsis and hepatic encephalopathy, and 9 died during the study, though no deaths were determined to be related to the study.
