Cell-Free DNA as a Prognostic Marker in Stage I Non Small-Cell
Lung Cancer Patients Undergoing Stereotactic Body Radiotherapy
A study published in the journal Biomarkers found that plasma cell-free DNA (cfDNA) is an promising prognostic biomarker of Stage 1 NSCLC.
The researchers evaluated whether plasma cell-free DNA (cfDNA) was related to clinical outcome in inoperable stage I non-small cell lung cancer (NSCLC) patients undergoing stereotactic body radiotherapy (SBRT). The study was conducted by Maria Teresa Bortolin and others of CRS4 Centro di Ricerca, Sviluppo e Studi Superiori in Sardegna, Italy.
The researchers assessed plasma cfDNA at baseline, before the last day of SBRT, and 45 days after the end of SBRT, in 22 NSCLC patients. Patients’ results were compared with 22 healthy controls who were also evaluated.
Bortolin and others found that plasma cfDNA was higher in patients than in controls. “An association with unfavourable disease-free survival was found for continuous baseline cfDNA increments (HR = 5.9, 95%CI: 1.7–19.8, p = 0.04).” the researchers wrote. “Plasma cfDNA may be a promising prognostic biomarker in high-risk NSCLC patients.”
Lung Excision of Non-Small-Cell Lung Cancer Leaves Cancer Cells
In Residual Lobe: Cytological Detection Using Pulmonary Vein Blood
Inappropriate lung resection may leave cancer cells in the residual pulmonary lobe. Surgeons should resect as much pulmonary parenchyma as possible in the cancerous lung. Surgical margins should be equal to or greater than the size of the tumor.
“Our findings indicate the possibility of cancer cells remaining in the residual lobe after a wedge resection for NSCLC. In addition, the presence of cancer cells in the resected pulmonary lobe may be an indicator of later recurrence,” wrote Sawabata et al, in the journal Interactive CardioVascular and Thoracic Surgery.
"Inappropriate lung resection may leave cancer cells in the residual pulmonary lobe," Dr. Sawabata to MDalert.com.
"Surgeons should resect the pulmonary parenchyma as much as possible in excision of the lung with cancer. The milestone for little cancer cell leaving is the margin distance to the tumor grater than the size of tumor," Dr. Sawabata advised.
The study included 28 patients with pathological stage I NSCLC who underwent lung excision followed by a lobectomy were evaluated according to the status of isolated tumour cells (ITCs) (origin of circulating tumour cells) in PVB from the resected lobe. Survival was also assessed according to the status of ITCs.
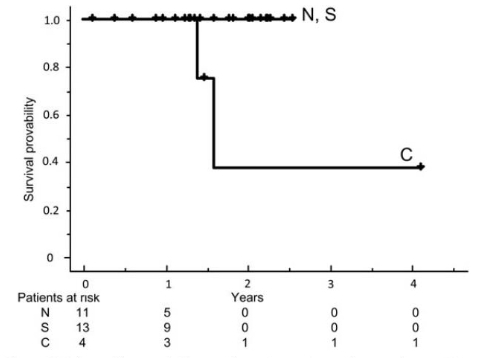
Figure 1. Relapse-free survival curves for patients who underwent lung excision followed by lobectomy. The 2-year relapse-free survival rate was 100% for patients with no residual tumor cells (N), 100% for those with singular cells (S) and 37.5% for those with clustered cells (C) in pulmonary vein blood.
Contamination of Health Care Personnel
During Removal of Personal Protective Equipment
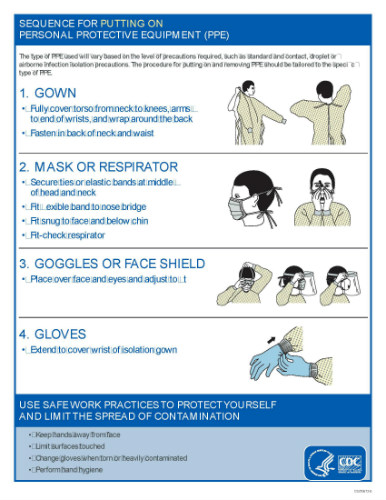
A study published online in JAMA recently reports that “Contamination of the skin and clothing of healthcare personnel occurs frequently during removal of contaminated gloves or gowns. Educational interventions that include practice with immediate visual feedback on skin and clothing contamination can significantly reduce the risk of contamination during removal of personal protective equipment.”
"Knowing the correct way to don and doff PPE is extremely important because healthcare personnel can become contaminated with pathogens if they do this incorrectly," said Myreen Tomas, MD, an infectious disease specialist at the Cleveland Veterans Affairs Medical Center.

"Such contamination can place them at risk, as seen by recent cases of healthcare personnel acquiring Ebola virus infection," Dr Tomas told Medscape Medical News.
The study was overseen by led by Myreen Tomas, MD, an infectious disease specialist at the Cleveland Veterans Affairs Medical Center, recruited these volunteers from four hospitals in the Cleveland area.
The authors of the JAMA study reported employing an intervention to reduce the contamination rate of personal protective equipment (PPE). The intervention has been advocated by the Centers for Disease Control and Prevention (CDC).
Of 435 glove and gown removal simulations, contamination of skin or clothing with fluorescent lotion occurred in 200 (46.0%), with a similar frequency of contamination among the 4 hospitals (range, 42.5%-50.3%). Contamination occurred more frequently during removal of contaminated gloves than gowns (52.9% vs 37.8%, P = .002) and when lapses in technique were observed vs not observed (70.3% vs 30.0%, P < .001). The intervention resulted in a reduction in skin and clothing contamination during glove and gown removal (60.0% before the intervention vs 18.9% after, P < .001) that was sustained after 1 and 3 months (12.0% at both time points, P < .001 compared with before the intervention). During simulations of contaminated glove removal, the frequency of skin contamination was similar with fluorescent lotion and bacteriophage MS2 (58.0% vs 52.0%, P = .45).
Clearly the intervention reduces the contamination rate, but even when properly executed 30% of healthcare providers were contaminated. “The results help explain why multidrug-resistant bacteria are such a stubborn threat in hospitals,” wrote Karen Kaplan in the Los Angeles Times.
Decision to Adopt Medical Technology under the National Health Insurance System in Taiwan: Case Study of New Molecular Targeted Drugs among NSCLC patients.
An article in the Journal of Evaluation in Clinical Practice by HL Chen et al reports on the decision to adopt medical technology under the national health insurance system in Taiwan. Chen reports on a case study of new molecular targeted drugs among NSCLC patients.
Molecular targeted drugs (MTD), have been proven to provide clinical benefits to advanced stage non-small cell lung cancer (NSCLC) patients. Therefore, access to such medical innovations in time is critical for patients with the right indications. The aim of this study was to explore determinants of the adoption of MTD among NSCLC patients under Taiwan's National Health Insurance (NHI) system.
Using Taiwan's Longitudinal Health Insurance Database and Cancer Registry database as the data source, the researchers identified 1555 newly diagnosed NSCLC patients who started cancer treatment between 2004 and 2009. Patients were categorized into non-MTD and MTD groups based on the cancer treatment they received.
Hierarchical logistic regression was used to explore potential determinants associated with the adoption of MTD by adjusting for patient-, disease-, doctor-, hospital-level characteristics and changes of reimbursement schemes.
During the study period, 562 (36%) NSCLC patients were classified as the MTD group and 993 (64%) patients were the non-MTD group. Hierarchical logistic regression model showed that the elderly were less likely to receive MTD (OR = 0.41; 95% CI: 0.28-0.60).
In contrast, patients whose cancer type was adenocarcinoma (OR = 2.99; 95% CI: 2.09-4.26) were more likely to receive MTD. Those who went to private hospitals (OR = 1.75; 95% CI: 1.01-3.03) and hospitals with higher economic scale (OR = 3.00; 95% CI: 1.72-5.25) were more likely to receive MTD as well.
“Our findings suggest that both patient- and hospital-level characteristics significantly affected the adoption of MTD among NSCLC patients,” the researchers concluded.
