Keep current with the literature. Take a look at these 5 studies that will change the course of oncology in general, and the experience of patients with non-small cell lung cancer (NSCLC) in particular. The advances in the progress in cancer therapy continue at a rapid rate.
Here is a list of summaries of the main findings, along with links to more information.
1. Adjuvant Chemotherapy Improves NSCLC Survival
Adjuvant chemotherapy improves survival in all patients with non-small cell lung cancer, according to a recent report in the Journal of Surgical Oncology. The effects were evident in both female and male patients.
“Adjuvant chemotherapy appears to increase survival for patients with resected NSCLC tumor larger than 4 cm. Women with NSCLC experience improved survival relative to men regardless of treatment,” the authors reported.
The researchers collected data from the National Cancer Data Base on adults diagnosed with NSCLC who underwent lobectomy with or without adjuvant chemotherapy for pathologic T2 tumors measuring ≥4 cm, with no lymph node involvement or distant metastasis. Patients who underwent chemotherapy following surgery experienced a survival benefit compared with patients who were treated with surgery alone (5-year survival of 66 vs. 49 %, P < 0.0001), according to the report.
Overall, women had improved 5-year survival relative to men (60% vs. 47%, P < 0.0001), though the clinical picture is somewhat more complex. By contrast, all groups of men identified by recursive partitioning analysis demonstrated improved survival with adjuvant chemotherapy. Adjuvant chemotherapy appears to increase survival for patients with resected NSCLC tumor larger than 4 cm. Women with NSCLC experience improved survival relative to men regardless of treatment.
2. A Prognostic Model to Predict Mortality Among Non-Small Cell Lung Cancer Patients in the U.S. Military Health System
A study reported recently in the Journal of Thoracic Oncology described an effective prognostic model patients with NSCLC.
These researchers used the linked database from the Department of Defense's Central Cancer Registry (CCR) and the Military Health System Data Repository (MHS).
“A simple risk scoring system was developed to aid quick risk score calculation and risk estimation for NSCLC clinical management. The study subjects were 5,054 patients diagnosed with NSCLC between 1998 and 2007. Age, sex, tobacco use, tumor stage, histology, surgery, chemotherapy, peripheral vascular disease, cerebrovascular disease and diabetes mellitus were identified as significant predictors of survival. Calibration showed high agreement between predicted and observed event rates. The AUC reached 0.841, 0.849, 0.848, and 0.838 over one, two, three and five years, respectively.”
This is the first NSCLC prognosis model for quick risk assessment within the MHS.
3. Clinical Trials Integrating Immunotherapy and Radiation for Non-Small-Cell Lung Cancer
A second study to appear recently in the Journal of Thoracic Oncology explores the efficacy of immunotherapy combined with radiotherapy in the treatment of NSCLC.
“With overall response rates less than 20%, combinatorial strategies that extend the benefit of these agents to more patients are desirable. The integration of radiotherapy with immunotherapy is a conceptually promising strategy, as radiotherapy has potent immunomodulatory effects and may contribute not only to local control but may also augment systemic antitumor immune response. Preclinical data and case reports suggest the potential for robust clinical responses in metastatic NSCLC patients using this strategy, but prospective clinical trials evaluating the integration of radiation and immunotherapy are limited. The use of immunotherapy in non-metastatic settings is also intriguing but understudied. We review the potential clinical settings of interest for the partnering of immunotherapy and radiation in NSCLC, including early stage, locally advanced, and metastatic disease, and review completed, accruing, and developing clinical trials.
4. Overall Survival Benefits of First-Line EGFR Tyrosine Kinase Inhibitors in EGFR-Mutated Non-Small-Cell Lung Cancers: A Systematic Review and Meta-Analysis
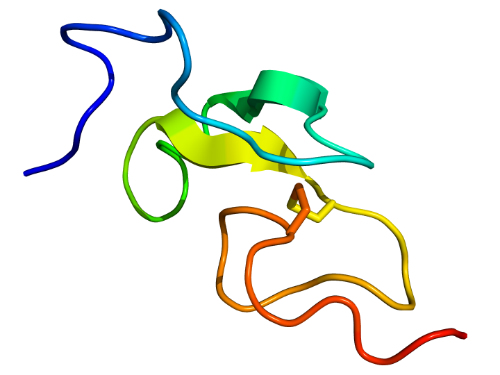
“In patients with advanced NSCLC harboring exon 19 deletions, tyrosine kinase inhibitors (TKIs) are associated with improved overall survival compared to those patients receiving conventional chemotherapy,” according to a report in the British Journal of Cancer.
“Accumulating data shows that exon 19 deletions and L858R, both activating epidermal growth factor receptor mutations in non-small-cell lung cancers (NSCLCs), are just 2 different entities in terms of prognosis and treatment response to tyrosine kinase inhibitors (TKIs).”
This systematic review and meta-analysis of randomized controlled trials comparing TKIs with conventional chemotherapy included 8 trials and 1498 patients. Additionally, 5 trials of 1279 patients with either exon 19 deletions or L858R were included in the meta-analysis.”
5. HPV-Related Cancers Will Us Hit Hard
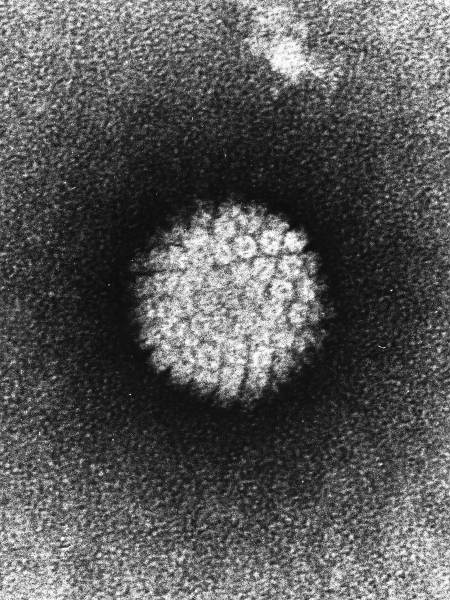
According to an upcoming publication in Hematology and Oncology Clinics of North America, human papillomavirus (HPV) is going to be a serious problem for oncologists over coming decades.
The researchers from The Ohio State University wrote “Human papillomavirus (HPV) is a common sexually transmitted infection that is the cause of a distinct subset of oropharyngeal cancer (OPC) rising in incidence in the United States and other developed countries.”
This increased incidence, combined with the strong effect of tumor HPV status on survival, has had a profound effect on the head and neck cancer (HNC) discipline.
The multidisciplinary field of HNC clinicians is in the midst of re-evaluating evidence-based algorithms for clinical decision making, developed from clinical trials conducted in an era when HPV-negative cancer predominated.
This article reviews “relationships between tumor HPV status and gender, cancer incidence trends, overall survival, treatment response, racial disparities, tumor staging, risk stratification, survival post disease progression, and clinical trial design.”
It also offers clinicians a future scenario where the thousands of current HPV infections convert to head and neck cancers over the next 20 to 30 years.
